In this Article
Gallstones
What Are Gallstones?
Gallstones are collections of hard, solid material that form in the gallbladder. Some may be the size of a grain of sand, or they may be crystals that can be seen only with a microscope. Others may be the size of a golf ball. People can develop just one large stone, hundreds of smaller stones, or combinations of both.
- The medical name for gallstones is cholelithiasis (KOL-e-lee-thigh-e-sis).
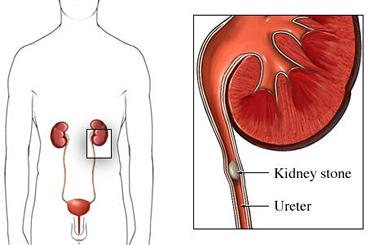
- Gallstones are one of several kinds of stones, or calculi, that can form in the body.
- Stones also develop in other hollow organs or ducts in the body. Kidney stones, for instance, may occur in the kidneys, urinary bladder, or urinary ducts.
What Is The Gallbladder?

The gallbladder is a hollow, pear-shaped organ with tough, muscular walls. It is located in the upper right-hand part of the
- Bile is a digestive juice that helps the body digest fats.
- The liver makes about 3 cups of bile each day.
- Bile flows from the liver, where it is made, into the gallbladder, where it is stored, through the hepatic ducts, which are tubes connecting the liver to the gallbladder.

The gallbladder stores bile until it is needed for digestion. Right after each meal, the gallbladder’s muscular walls contract, squeezing bile out through the
When digestion is done, and no more food is in the small intestine, the gallbladder relaxes, collects more bile, and waits for the next meal.
How Do Gallstones Form?
Bile consists of solid materials dissolved in liquid, much like sugar or salt dissolve in water. The materials include
- Most gallstones form when there is too much cholesterol in the bile. Cholesterol drops out of the liquid part of bile, just like too much sugar or salt will form crystals at the bottom of a glass of water. The tiny crystals of cholesterol group together to form the larger masses called gallstones.
- Cholesterol stones also can form when the gallbladder does not empty normally, and the bile is stored for long periods of time. About 80% of people with gallstones in the U.S. have cholesterol stones.
- Some gallstones form from bilirubin, a pigment the liver removes from blood as old red blood cells die and break apart. They are called “pigment stones.”
- Individuals also can have “mixed” stones, mixtures of cholesterol, bilirubin, calcium, and other material.
|
Facts About Gallstones
|
What Are The Symptoms Of Gallstones?
Gallstones may cause no symptoms at all or may cause various symptoms, sometimes severe.
Most gallstones don’t cause illness and are termed “silent” stones. They often are discovered accidentally, when an individual has medical tests for other health concerns. Silent gallstones may be small enough to pass through the ducts between the liver and small intestines, and out of the body. Silent stones also may be quite large, but they remain in the gallbladder and never move.

Gallstones cause trouble when they:
- Irritate the gallbladder, causing a condition called cholecystitis. When gallstones partially block the flow of bile out of the gallbladder, bile remaining in the gallbladder becomes stronger or more concentrated. That irritates the bladder walls, causing inflammation.
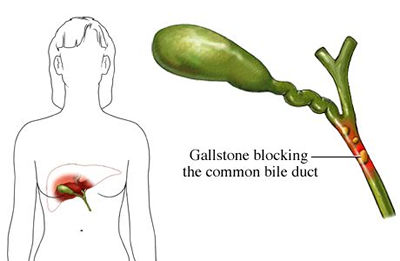
- Get stuck in ducts that carry bile from the liver to the small intestine, causing sudden severe pain called biliary colic.
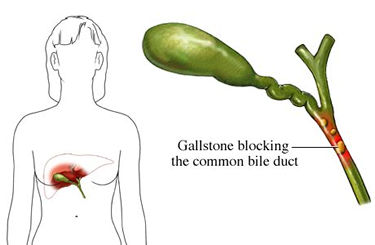
Gallstones may get stuck in:

- Hepatic ducts, which carry bile out of the liver.
- The cystic duct, which carries bile to and from the gallbladder.
- The common bile duct, which collects bile from the cystic and hepatic ducts and carries it to the small intestine.
- Doctors gave the common bile duct its name because it is shared by several organs, which use it in common. A duct from the pancreas also opens into the common bile duct. It carries digestive juices containing powerful enzymes from the pancreas to the small intestine.
- A gallstone that blocks the opening of the pancreatic duct may cause digestive enzymes to become trapped inside the pancreas. The result can be a very painful and dangerous inflammation of the pancreas called pancreatitis.

|
Symptoms of Jaundice Abdominal pain, nausea, vomiting, and a bloated feeling in the stomach and chest are the most common symptoms of a gallstone attack. Similar symptoms can occur in a number of serious diseases, including a heart attack. They also can occur in ordinary indigestion. When the symptoms occur, it is important to get medical advice. A gallstone attack can be very painful.
|
Many people who have a gallstone attack recall similar but less severe symptoms that occurred in the past, but disappeared. Those probably were due to small gallstones that lodged briefly in the ducts and then passed into the small intestine
Gallstones And Jaundice
If gallstones pass into the common bile duct, they may become stuck at the lower end of the duct and prevent the free flow of bile into the intestine. When the flow of bile is blocked, it backs up into the liver and spills over into the blood. This results in jaundice.
Jaundice is a yellowing of the skin and the whites of the eyes. The urine turns dark and the stools become a pale clay color, instead of brown. These color changes are due to the high bile pigment concentration in the blood. The condition is called obstructive jaundice because an obstruction in the bile duct – the gallstone – is the cause.
Sometimes a stone will become unstuck and pass into the intestine. Then jaundice improves. Often, however, the stone simply “uncorks” temporarily and stays in the common bile duct, where it may block bile flow again in the future.
If the stone remains stuck in the duct, the jaundice will worsen. This may become life threatening:
- Individuals with obstructive jaundice often are very ill and need emergency surgery to remove the gallstone reopen the duct.
- Without surgery, they face a high risk of infections, serious complications and death.
- Obstructive jaundice often occurs in elderly people who are less able to cope with the complications.
- The risk of obstructive jaundice is one important reason why people with gallstone symptoms usually should have their gallbladder removed.
- Fortunately, only a very small percentage of people with gallbladder disease develop jaundice.
Who Is At Risk For Gallstones?
Cholesterol stones form in people who have an imbalance in the materials that make-up bile.
- There may be too much bilirubin and cholesterol, or not enough bile salts, compared to the amount of water in the bile. (Bile salts help to keep cholesterol dissolved in the bile.)
- Cholesterol stones also may form when the gallbladder does not empty normally, and the bile stands for long period of time.
- Pigment stones develop most often in people with cirrhosis, an inflammation of the liver; infections of the gallbladder; or inherited blood diseases, such as sickle cell anemia.
Several other factors increase the risk for gallbladder disease:
- Gender. Women between the ages of 20 and 40 are twice as likely to get
gallstones than men are. Estrogen, the female sex hormone, increases the amount of cholesterol in the bile. Extra estrogen from birth control pills or hormone replacement therapy may further increase bile’s cholesterol content. It also may slow gallbladder emptying, allowing bile to stand for longer periods of time. - Pregnancy. Estrogen levels increase during pregnancy. The risk may increase with the number of pregnancies, since women who have been pregnant several times are at especially high risk for gallstones.
- Obesity. Being overweight tends to reduce the amount of bile salts in bile, so that less cholesterol can stay dissolved. Obesity also slows the rate at which the gallbladder empties. Some studies suggest that being even moderately overweight can increase the risk of gallstones.
- Rapid weight loss. “Crash diets” and fasting make the body burn, or metabolize, fat very rapidly. The liver reacts by releasing extra cholesterol into the bile. Fasting slows gallbladder emptying, since no food is present in the
small intestine to signal the need for bile. - Age. Although gallstones occur in younger people, especially women, most cases are diagnosed in people over age 60.
- Ethnic heritage. Native Americans have the highest rate of gallbladder disease in the U.S. Mexican-Americans also have an unusually high risk. Scientists believe these groups have a genetic tendency to produce bile with large amounts of cholesterol.
- Taking cholesterol-lowering drugs. Drugs that lower blood cholesterol may increase the amount of cholesterol passed out of the body in the bile.
How Are Gallstones Diagnosed?
Accurate diagnosis is very important because gallstone symptoms are similar to those of several serious diseases.
They include heart attacks, ulcers, appendicitis, pancreatitis, hiatal hernia, and hepatitis.
Doctors may suspect gallstones based on a person’s symptoms, especially in someone who is at high risk for gallbladder disease. A simple physical examination in the doctor’s office may also suggest gallbladder disease. The doctor, for instance, usually presses gently with his fingers just below the ribs on the right side of the chest. That area often is tender in people with gallbladder disease. Blood tests also can show signs of obstructed ducts.
Two tests can diagnose most cases of gallbladder disease with great accuracy, an abdominal ultrasound and oral cholecystogram (OCG) or cholescintigraphy.
Ultrasound
An
The sound waves bounce off the gallbladder,
An ultrasound scan can provide a great deal of information about a person’s condition by:
- Confirming whether gallstones are present
- Showing how many stones are present, and their size
- Seeing whether the stones are in the gallbladder or the ducts
Ultrasound scans
- Are painless
- Do not involve x-rays or use of radioactive materials
- Have no known damaging effects on the body
- Can be repeated safely as many times as needed
For further information about ultrasound, go to Ultrasound.
Oral Cholecystogram Or Cholescintigraphy
An oral cholecystogram (OCG) or cholescintigraphy involves receiving an injection of an iodine x-ray dye into a vein, or taking iodine pills. X-rays then are taken of the gallbladder to see whether it contracts normally or stones are present.
Diagnosing Stones In The Common Bile Duct
Diagnosing stones that have passed into the
- ERCP (Endoscopic retrograde cholangiopancreatography)involves swallowing a thin, flexible tube, or
endoscope , that the doctor gently moves through the gastrointestinal tract to thesmall intestine . He releases a special dye into the small intestine, and it stains the gallbladder’s ducts. Any stones present in the ducts then can be seen on an x-ray. - PTC (Percutaneous transhepatic cholangiography) involves injecting x-ray dye into the bile ducts with a needle that is passed through the liver.
|
Nice To Know: Q. I had an ultrasound scan of the abdomen for another medical problem. It showed several big stones in my gallbladder. Should I have my gallbladder removed? A. About 60% of people with gallstones never have any symptoms and never get sick. They’re just like you. Most might never even know they had gallstones. Their stones are discovered by accident, during tests for other diseases. If you do start having abdominal pain after fatty meals, indigestion, gas, bloating, or other symptoms, make sure to remind the doctor about the ultrasound scan results. |
How Are Gallstones Treated?
Some people with gallstones have no symptoms, and may require no treatment. For individuals who are having symptoms, surgery to remove the gallbladder is the most common treatment.
Surgery to Remove the Gallbladder.
Surgery for Blocked Bile Ducts.
Surgery To Remove The Gallbladder
Surgery for gallstone disease is called
People can live normally without a gallbladder and do not need a change in diet or a special diet. When the gallbladder is removed, the
There are two ways of removing a diseased gallbladder. One is a newer laparoscopic or “Band-Aid” surgery, in which the surgeon inserts a narrow, long-handled tool, or
|
Nice To Know: Q. Two months ago, my wife went to the emergency room in the middle of the night with severe abdominal pain. The doctor said it was a gallstone attack, and recommended removal of her gallbladder. She’s had no more problems since then. Could the disease have just gone away? A. Some people do have just one gallbladder attack. But one attack carries about a 70% risk of having another. Your wife may be having symptoms, but confusing them with ordinary indigestion. If tests show that her gallbladder is infected or inflamed, immediate surgery may be necessary. Surgery also may be wise if there are more stones in her gallbladder or she does a lot of foreign travel, which could complicate a sudden need for surgery. Your wife should discuss her own situation with the doctor and find the best approach for her. |
Possible complications from gallbladder surgery: The most common and most serious is damage to the bile ducts that results in leakage of bile. It can cause a serious and painful abdominal infection. Infections sometimes can be treated with medication. In other cases, a second operation is needed to repair the leaking duct. These complications are not common.
Laparoscopic Surgery
This “minimally invasive” surgery was introduced in the U.S. in 1988. It now is the standard, or most commonly used, surgery. About 95% of gallbladder surgery is done in this way. It is called “minimally invasive” because the incisions are very small. Patients thus have less pain after surgery, shorter hospital stays, and can resume normal activities sooner. Scars from a laparoscopic cholecystectomy are barely visible.
- Surgery is done with a general anesthetic. In the operation, the surgeon makes several small incisions in the abdomen. The holes are used to insert instruments to perform the surgery.
- One incision is used to insert the laparoscope, a pencil-thin device that contains a miniature video camera, power light, and channels for inserting mini-surgical instruments. The camera sends a magnified image to a television monitor, giving the surgeon a clear view of internal organs.
- The surgeon watches the monitor image while locating the gallbladder, separating it from the liver, ducts, and other nearby structures. Then he uses mini-scissors, clamps, and other tools to detach the gallbladder from the liver and its other attachments. The gallbladder is removed from the body through one of the incisions.
- Patients receive pain medicine after awakening from the anesthetic. Pain, however, is not severe. Patients usually stay in the hospital only one night. They can start eating a normal diet the day after surgery. Most can resume normal daily activities 3 to 5 days after surgery.
Traditional “Open” Surgery
A traditional cholecystectomy is called “open” surgery because the surgeon removes the gallbladder through a 5-inch to 8-inch incision in the abdomen just below the ribs. Open surgery is done in only about 5% of cholecystectomies in the U.S.
|
Nice To Know: Open gallbladder surgery is now used mainly on patients who have gall bladder infections, internal scar tissue from previous abdominal operations, or other problems that make laparoscopic surgery unsuitable. Sometimes surgeons recognize these problems before the operation, and choose open surgery. In other instances, they encounter the difficulties after starting with the laparoscopic method, and switch to open surgery. |
- Although discomfort from open surgery is more severe, it can be relieved with pain medicine.
- With open surgery, patients usually must stay in the hospital for 2 to7 days.
- Patients often have to spend several weeks at home recovering before resuming normal activities.
Surgery For Blocked Bile Ducts
Patients with gallstones lodged in the bile ducts may need two-step surgery. That’s because removal of the gallbladder alone would not cure the disease. Rather, it would leave the ducts blocked by the stone, and symptoms would continue.
- In these cases, the surgeon may use ERCP to remove the gallstones from the duct. The method is similar to ERCP used to diagnose
gallbladder disease, but in this case the surgeon uses an instrument on theendoscope to cut the duct. He catches the stone in a tiny basket, and removes it with the endoscope. - ERCP may be done before removing the gallbladder, or during the cholecystectomy.
|
Nice To Know: Q. When my mom had gallbladder surgery, she stayed in the hospital for a week. It took her weeks at home to get back to normal. The doctor says modern surgery is a lot easier on patients. He says I need to stay just overnight, and can go back to work in about a week. Does that sound right? A. Today, most gallbladder operations are done with a “Band-Aid” method. It is called “minimally invasive” surgery because it uses small incisions, instead of the 6-inch to 8-inch incision used in the past. The doctor operates through a laparoscope, a pencil thin instrument with a mini-camera. Patients have less discomfort after surgery, heal faster, and resume normal activities sooner |
Non-Surgical Treatment
Non-surgical treatments for gallstones are available, but they have disadvantages. The alternative treatments, for instance, are not cures. Gallstones return in about half of people treated. Treatment also may require taking medicine for months or years while symptoms continue, and many trips to the doctor.
Alternative treatments include the following:
- Oral dissolution therapy involves taking oral drugs to dissolve gallstones. The drugs Chenix (chenodiol) and Actigall (ursodiol) work best for small stones made from
cholesterol .It takes time for drugs to dissolve gallstones. People often must stay on oral therapy for many months. In addition, treatment does not cure the underlying problem that caused gallstones. Thus when individuals stop taking the medicine, new gallstones may develop. The main side effect of drug therapy is mild diarrhea.
- Extracorporeal shockwave lithotripsy (ESWL) uses powerful shock waves produced by a medical instrument to break up gallstones. Stones are broken into pieces small enough to pass through the
common bile duct and into the small intestine.Attacks of
biliary colic may occur as the stones pass through the duct. ESWL can be used only for certain types of stones. In addition, it may fail to break up all the stones. In such cases, individuals sometimes can be treated with oral dissolution therapy. - Contact dissolution therapy is an experimental treatment being tested for safety and effectiveness. It involves injecting a chemical, methyl tert butyl ether, directly into the gallbladder to dissolve stones. The chemical can dissolve only cholesterol stones.
|
Nice To Know: Q. Why should I have my gallbladder removed when non-surgical treatments are available? A. Non-surgical treatments have plenty of disadvantages. One is that they usually are not a permanent cure. Drugs that dissolve gallstones, for instance, must be taken every day for months or years. They work for only certain kinds of gallstones. If you stop the medicine, gallstones usually start to form again. Shockwave therapy can break gallstones into pieces small enough to pass from the body. But it often doesn’t work, and patients may have to take drugs for the rest of their life to keep new stones from forming. |
What Is The Outlook For Gallbladder Disease?
Scientists are looking for more effective non-surgical treatments for gallbladder disease.
Drugs that dissolve gallstones quickly could reduce the need for surgery. Other research is under way on the prevention of gallstones.
Genes that children inherit from their parents may be a factor in many gallstone cases. If scientists can identify these abnormal genes, it would pave the way for gene therapy to replace the defective gene with a normal copy.
Meanwhile, research is under way on new surgical methods that are even less invasive than laparoscopic operations. These methods would involve use of mini-surgical instruments that further reduce the discomfort and recovery time for patients.
Gallstones: Frequently Asked Questions
Here are some frequently asked questions related to Gallstones.
Q: I had an ultrasound scan of the
A: About 60% of people with gallstones never have any symptoms and never get sick. They’re just like you. Most might never even know they had gallstones. Their stones are discovered by accident, during tests for other diseases. If you do start having abdominal pain after fatty meals, indigestion, gas, bloating, or other symptoms, make sure to remind the doctor about the ultrasound scan results.
Q: Two friends went on crash diets, and lost a lot of weight real fast. Within a few months, both developed gallstones and needed surgery. How could dieting cause gallstones?
A: Rapid weight loss diets and fasting do increase the risk for gallstones. Both tend to increase the amount of
Q: Will I need to stay on a special diet after having my gallbladder removed?
A: People can live normally without a gallbladder. Your
Q: Ever since gallbladder surgery, I’ve had looser bowel movements. I also have bowel movements more often now. Could removal of my gallbladder have caused digestive problems?
A: Almost 1 in every 3 people have looser and more frequent bowel movements after gallbladder surgery. A few develop more troublesome diarrhea. Scientists think that gallbladder removal decreases the amount of time that food remains in the large intestine. The large intestine removes water from digested food and stores
Q: Two months ago, my wife went to the emergency room in the middle of the night with severe abdominal pain. The doctor said it was a gallstone attack, and recommended removal of her gallbladder. She’s had no more problems since then. Could the disease have just gone away?
A: Some people do have just one gallbladder attack. But one attack carries about a 70% risk of having another. Your wife may be having symptoms, but confusing them with ordinary indigestion. If tests show that her gallbladder is infected or inflamed, immediate surgery may be necessary. Surgery also may be wise if there are more stones in her gallbladder or she does a lot of foreign travel, which could complicate a sudden need for surgery. Your wife should discuss her own situation with the doctor and find the best approach for her.
Q: Why should I have my gallbladder removed when non-surgical treatments are available?
A: Non-surgical treatments have plenty of disadvantages. One is that they usually are not a permanent cure. Drugs that dissolve gallstones, for instance, must be taken every day for months or years. They work for only certain kinds of gallstones. If you stop the medicine, gallstones usually start to form again. Shockwave therapy can break gallstones into pieces small enough to pass from the body. But it often doesn’t work, and patients may have to take drugs for the rest of their life to keep new stones from forming.
Q: When my mom had gallbladder surgery, she stayed in the hospital for a week. It took her weeks at home to get back to normal. The doctor says modern surgery is a lot easier on patients. He says I need to stay just overnight, and can go back to work in about a week. Does that sound right?
A: Today, most gallbladder operations are done with a “Band-Aid” method. It is called “minimally invasive” surgery because it uses small incisions, instead of the 6-inch to 8-inch incision used in the past. The doctor operates through a
Gallstones: Putting It All Together
Here is a summary of the important facts and information related to gallstones.
- Gallstones are made of hard, solid material that forms in the
gallbladder . - The gallbladder is a hollow organ that stores
bile , a thick liquid that helps the body digest fats. - Gallstones can block tube-like ducts that carry bile from the gallbladder to the
small intestine . - A blockage usually causes severe pain in the upper right part of the
abdomen , just below the ribs. - Gallstones can be permanently cured with surgery to remove the gallbladder.
- A fairly new operation for removing the gallbladder, sometimes called Band-Aid surgery, means less discomfort and a quicker recovery for patients.
Gallstones: Glossary
Here are definitions of medical terms related to Gallstones.
Abdomen: The stomach area that begins just below the ribs and extends to the pelvis.
Abdominal ultrasound scan: A test that uses sound waves to create images of organs inside the body. If gallstones are present in the gallbladder they will be seen..
Bile: A thick brown liquid made by the liver that helps the body digest fats. It is stored in the gallbladder and released when food enters the small intestine.
Bile salts: Chemicals present in bile that help in the digestion of fats and also keep cholesterol dissolved in the bile.
Biliary colic: A spasm-like pain caused when gallstones pass into the common bile duct.
Bilirubin: A material released into the blood when red blood cells break-down. It is present in the bile as a waste material to be eliminated from the body.
Cholelithiasis: The medical term for gallstones.
Cholescintigraphy: A test used to diagnose gallstones in which radioactive x-ray dye is injected into a vein to make stones visible to a nuclear imaging scanner.
Cholecystitis: An inflammation of the gallbladder.
Cholecystectomy: Surgical removal of the gallbladder to treat gallstones.
Cholesterol: A fatty material necessary for many body processes. It is present in bile as a waste material. Most gallstones are made from cholesterol.
Cirrhosis: An inflammation of the liver that can increase the risk of certain kinds of gallstones.
Common bile duct: The duct that collects bile from the liver and gallbladder, as well as digestive juices from the pancreas, and carries them to the small intestine.
Cystic duct: The tube that carries bile to and from the gallbladder.
Endoscope: A thin, flexible tube that a patient swallows that allows the physician to see inside the upper gastro-intestinal tract. A camera is attached to the outer end. The surgeon may perform some procedures like removing gallstones using a tiny basket on the end of the instrument.
Endoscopic retrograde cholangiopancreatography(ERCP): A procedure used to diagnose and sometimes remove gallstones blocking the common bile duct. It involves swallowing an endoscope, which the doctor gently moves through the gastrointestinal tract to the small intestine. A special dye is released into the small intestine so that gallstones can be seen on x-ray. This technique can be adapted for use in surgery to remove gallstones using a tiny basket attached to the end of the endoscope.
Extracorporeal shockwave lithotripsy (ESWL): A procedure in which powerful shock waves produced by a medical instrument are used to break up gallstones into pieces small enough to pass through the common bile duct and into the small intestine.
Feces: Stool; undigested food and other waste stored in the large intestine until it is eliminated from the body.
Gallbladder: The pear-shaped organ located in the right side of the abdomen that stores and releases bile.
Gallstones: Stone-like objects that form from cholesterol and other substances in the bile. They may be as small as tiny crystals or as large as golf balls.
Hepatic duct: The tube that collects bile from the liver and delivers it to the gallbladder.
Hiatal hernia: A condition that occurs when part of the stomach bulges through the sheet of tissue that separates the chest cavity from the abdomen.
Jaundice: an often serious condition in which the skin and whites of the eyes become yellowish. If due to a gallstone that blocks the flow of bile through the common bile duct it is called obstructive jaundice.. There are other causes of jaundice not associated with gallstones.
Laparoscope: A pencil-thin instrument used for minimally invasive, or Band-Aid, surgery.
Liver: A large organ in the upper right side of the abdomen that has many important functions, including making bile and cholesterol.
Oral cholecystogram (OCG): A test used to diagnose gallstones that involves taking an iodine pill that makes stones visible on x-rays.
Pancreas: An organ that produces digestive juices. It sometimes can become inflamed in people with gallstones.
Pancreatitis: A potentially dangerous inflammation of the pancreas that can occur in people with gallstones.
Percutaneous transhepatic cholangiography(PTC): A procedure that involves injecting dye into the bile ducts with a needle that is passed through the liver so that gallstones can be seen on x-ray.
Small intestine: The part of the digestive tract where food passes from the stomach and is broken down into nutrients that the body can absorb and use.
Gallstones: Additional Sources Of Information
Here are some reliable sources that can provide more information on gallstones.
National Digestive Diseases Information Clearinghouse
www.niddk.nih.gov/health/digest/nddic.htm
American Gastroenterological Association
Phone: 301-654-2055
www.gastro.org
National Institute of Diabetes & Digestive & Kidney Diseases Office of Communications and Public Liaison
www.niddk.nih.gov
