In this Article
Hypothyroidism
What Is Hypothyroidism?
Hypothyroidism is a condition in which there is too little thyroid hormone in the bloodstream. The thyroid gland, which produces the thyroid hormones, is said to be “underactive,” because it does not produce enough thyroid hormone for the body to function normally.

Inadequate production of thyroid hormone affects stimulation of cells and organs in the body. The low level of thyroid hormone causes the symptoms associated with hypothyroidism, which is generally a “slowing-down” of the body’s processes. These symptoms include slowed heart rate, tiredness, inability to tolerate cold, mental fatigue, and constipation.

Hypothyroidism is a common condition, and it can be successfully treated. However, the symptoms are often subtle. People may believe their symptoms are due to stress, depression, or “getting older.” Frequently, they may mistake the signs and symptoms of hypothyroidism for other conditions. It is not unusual for someone with hypothyroidism to go undiagnosed, sometimes for many years. Some experts estimate that as many as 9 million people in the U.S. have undiagnosed hypothyroidism.
Low thyroid levels can affect both men and women, but it is far more common in women.
|
Need To Know: A different thyroid-related condition involves too much thyroid hormone in the bloodstream, producing symptoms that include rapid heart beat, extreme fatigue, weight loss, and nervousness. This condition is called For further information about hyperthyroidism, go to Hyperthyroidism. |
|
Nice To Know: What is the thyroid gland? The thyroid gland is a small, butterfly-shaped gland that lies just under the The thyroid gland secretes thyroid hormones, which control the speed at which the body’s chemical functions proceed (metabolism). To produce thyroid hormones, the thyroid gland needs |
What Is Thyroid Hormone?
Hormones are chemical messengers released into the bloodstream by specialized glands called endocrine glands. A hormone circulates through the body in the bloodstream, delivering messages to other parts of the body. The “message” causes effects far from the gland that produced the hormone.
Thyroid hormone is produced in the thyroid gland, which is located in the front of the neck. It is released by the thyroid gland into the bloodstream and circulates throughout the body. Almost every cell in the body, from those in the brain to those in the feet, responds to the hormone.
There are two different forms of thyroid hormone present in the bloodstream. The two forms of thyroid hormone differ in the number of iodine units or atoms attached to the hormone. Iodine is a very important component of thyroid hormone.
- Thyroid hormone with four iodine units is abbreviated as
T4 . - Thyroid hormone with three iodine units is abbreviated as
T3 . - Most thyroid hormone in the blood is T4.
- T3 is the form that is active in the body. T4 is inactive.
- Certain cells in the body convert T4 to T3.
|
Nice To Know: Just about all the iodine we consume in food is used by the body for the production of thyroid hormone.
In developed countries, iodine is added to regular table salt to ensure that individuals get enough iodine in their diets. Salt boxes are usually labeled “iodized salt.” In underdeveloped countries, there are nearly 200 million people with goiters (enlarged thyroids) due to insufficient iodine in their diet. |

What Does Thyroid Hormone Do?
Cells respond to thyroid hormone with an increase in the rate at which they burn energy, called metabolic activity. Metabolic activity, or metabolism, is a term used to describe the processes in the body that produce energy and the chemical substances necessary for cells to grow, divide to form new cells, and perform other vital functions.
If you think of each cell in the body as a motor car, then thyroid hormone acts as if you were tapping on the accelerator pedal. Its message is “Go!”
Because
- Heart rate increases.
- Breathing rate increases.
- Use of proteins, fats, and carbohydrates rises.
- Skeletal muscles work more efficiently.
- Muscle tone in the digestive system, such as those in the walls of the intestines that help to move food through the digestive system increases.
- Mental alertness and thinking skills are sharpened.

How Are the Blood Levels of Thyroid Hormone Controlled?
Normally, levels of thyroid hormone are regulated so that the body runs like a car on cruise control, functioning at a steady rate. This steady state is known as homeostasis. Here’s how the body’s control system regulates the cells to function at a steady, appropriate metabolic rate:
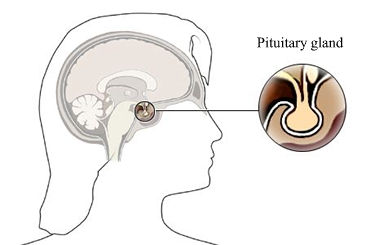
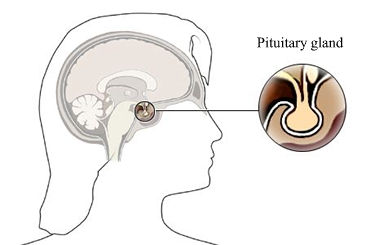
- Special “detector” cells in the brain monitor the level of thyroid hormone in the blood.
- When the level of thyroid hormone drops, these cells send signals to a nearby organ in the brain known as the
pituitary gland . - These signals stimulate the pituitary gland to release a substance called thyroid-stimulating hormone (TSH) into the bloodstream.
- TSH signals cells in the thyroid gland to release more thyroid hormone into the bloodstream.
- When the blood level of thyroid hormone has increased enough, the detector cells in the brain detect the increase in thyroid hormone level.
- These detector cells send signals to the pituitary gland to stop release of TSH.
|
Nice To Know: The medical specialty called |
|
Facts about hypothyroidism
|
What Are The Symptoms Of Hypothyroidism?
Symptoms of hypothyroidism usually appear gradually, particularly in people over age 50.

A low level of thyroid hormone slows the body’s metabolism, like running a motor car at a slow speed.
- Most symptoms, such as lower heart rate, tiredness, poor memory or difficulty in thinking, even constipation, are due to inadequate stimulation of the various organs in the body due to insufficient amounts of thyroid hormone.
- Other symptoms, such as inability to tolerate cold environments, are directly due to the decrease in heat generated within the body by slowed metabolic activity.
Most people with hypothyroidism will experience some of the following symptoms.
- Slow heart rate
- Tiredness
- Inability to tolerate cold
- Weight gain (usually 5 to 10 pounds)
- Emotional depression
- Drowsiness, even after sleeping through the night
- Heavy or irregular menstrual periods (in premenopausal women)
- Muscle cramps
- Constipation
Later symptoms of hypothyroidism include:
- Dry, flaky skin
- Hair loss
- Impaired memory and difficulty in thinking
- Voice becomes deeper
- A numb sensation in the arms and legs
- Puffiness in the face, especially around the eyes (a condition called myxedema, which is an indication that the disease has become serious)
|
Need To Know: It’s easy to dismiss symptoms such as feeling tired or being constipated as a part of aging, or as being linked to stress, which is why so many individuals with hypothyroidism remain undiagnosed. |
Who Gets Hypothyroidism?
Hypothyroidism can develop at any point in the life span. It is more common in adults, but hypothyroidism in infants and children also can occur.
- Women are three to eight times more likely than men to develop
Hashimoto’s thyroiditis , which can cause hypothyroidism. - The risk increases with age. By the time is woman reaches age 60, she has a one in five chance of having hypothyroidism.
- Thyroid disease can run in families. Sometimes it skips a generation, which means a person’s parents may have no sign of thyroid disease, though one of his or her grandparents may have had it.
- Individuals with insulin-dependent diabetes and rheumatoid arthritis have a higher chance of hypothyroidism.
- Hypothyroidism may occur in people with other autoimmune diseases such as Addison’s disease and
pernicious anemia . - It may occur in people with prematurely gray hair (before the age of 30) or those who have a skin condition known as
vitiligo , in which the normal pigmentation of the skin is lost and appears as white patches that do not tan normally in the sun. - Individuals with certain health conditions, who have had certain medical treatments, or who have taken certain medications also are more likely to develop hypothyroidism.
What Causes Hypothyroidism?
The vast majority of cases of hypothyroidism (roughly 95% or more) are caused by a problem within the thyroid gland. A much smaller number of cases (roughly 5% or less) are caused by a problem in the brain or pituitary gland, a small gland located beneath the brain.
The causes of hypothyroidism include:
- A condition called Hashimoto’s thyroiditis
- Treatment of hyperthyroidism
- Treatment of thyroid tumors
- Radiation
- Interference from drugs
- Subacute thyroiditis
- Postpartum thyroiditis
- Problems in the pituitary gland
Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is a condition resulting from a problem in the body’s
It is the most common cause of hypothyroidism.
The immune system is a complex network that normally defends the body against “invading” organisms and other foreign substances. When the immune system detects a foreign substance in the body, it responds to this by producing antibodies against the invaders. These antibodies will recognize and attack this foreign substance when they next encounter
In Hashimoto’s thyroiditis the immune system mistakenly directs an immune “attack” against its own healthy cells. Antibodies are manufactured and misdirected against the thyroid gland.
Any condition in which the body’s immune system attacks its own cells is called an auto-immune disease.
Inflammation associated with the abnormal immune response causes continuing loss of thyroid cells. Eventually, this loss in function (which may take months or even years) reaches the level where there is insufficient
Hashimoto’s thyroiditis is more common in women than in men (roughly 7 to 1), and it typically develops in women over age 40 years. It may be much more common than previously thought in older adults. Studies have indicated that up to 15 percent of women over age 60 years have evidence of mild hypothyroidism due to Hashimoto’s thyroiditis.
Because genetic factors can make someone vulnerable to developing autoimmune disease, it is not uncommon for persons with Hashimoto’s thyroiditis to have a history of other autoimmune disorders, including
In addition, the same genetic vulnerability toward disease means that more than one member of a family may develop Hashimoto’s thyroiditis or another
In the early stages of Hashimoto’s disease, inflammation causes the thyroid to become enlarged and rubbery, and this may be enough to be noticeable. Indeed, diagnostic blood testing may be done because a doctor notices an enlarged thyroid during a physical examination.
Blood testing typically shows low levels of the thyroid hormones
Treatment Of Hyperthyroidism
The treatment of hyperthyroidism – the condition in which the thyroid gland is “overactive” because there is too much thyroid hormone in the blood – can result in hypothyroidism. This can happen if:
- The hyperthyroidism was treated with
radioactive iodine . Nearly 50 percent of individuals who receive radioactive iodine for the treatment of hyperthyroidism from Graves’ disease will develop hypothyroidism within a year, and 65 percent will develop it within five years. - Most of the thyroid gland was removed surgically in order to treat the hyperthyroidism.
Treatment Of Thyroid Tumors
Surgery for a noncancerous (benign) or cancerous (malignant) thyroid tumor is another common cause of hypothyroidism.
- If the tumor is noncancerous, usually only a portion of the thyroid is removed, and hypothyroidism does not usually occur, unless most of the gland was removed.
- If the tumor is cancerous, usually the entire thyroid is removed.
In either case, hypothyroidism may develop at the time of treatment or a number of years afterward.
Radiation Treatment For Head And Neck Cancers
Exposure to high doses of radiation for the treatment of head and neck cancers also can cause hypothyroidism. Hypothyroidism may occur in up to 65% of such individuals within 10 years of the radiation treatment.
Interference From Drugs
Some drugs given for nonthyroid conditions have the side effect of inhibiting production of thyroid hormone within the thyroid gland. If these drugs are taken in large dosages or for a long time, hypothyroidism may result.
- Use of lithium as a treatment for certain psychiatric conditions is an example of drug-induced hypothyroidism. Almost half of all people who take lithium may develop an enlarged thyroid, although less than a quarter of them will actually develop symptoms of hypothyroidism.
- Another example is use of the iodine-containing drug amiodarone (Cordarone) for heart arrhythmias.
- In addition, drugs used in treatment of hyperthyroidism (propylthiouracil, for instance) can also impair thyroid function and cause hypothyroidism.
|
Need To Know: Numerous medications can affect the thyroid. Anyone who is at higher risk for |
Subacute Thyroiditis
Subacute thyroiditis is an inflammatory thyroid condition of unclear origin. It usually causes only temporary and mild hypothyroidism – that is, it produces a relatively less serious form of hypothyroidism that goes away on its own.
Subacute thyroiditis is an uncommon disorder that can occur in men or women of any age. The characteristic inflammation in the thyroid often follows an upper respiratory infection, and patients often come to a doctor’s attention because of noticeable and painful enlargement of the thyroid gland.
Postpartum Thyroiditis
Postpartum thyroiditis means inflammation of the thyroid following pregnancy, (from post, meaning “after,” and partum, meaning “birth”). It occurs in the first six months after delivery in about 5% to 9% of women. Typical symptoms relate to an initial phase of hyperthyroidism (with symptoms of rapid heart rate, increased sweating, nervousness) and a later phase of hypothyroidism (with fatigue, dry skin, feeling cold, depression).
Studies have shown that 80% to 90% or more of affected women had detectable levels before or during their pregnancies of antibodies directed against the thyroid gland.
- In up to 5% of women, this can cause inflammation of the thyroid up to 12 months after the delivery.
- Roughly 20% to 33% of the women who develop postpartum thyroiditis will have permanent hypothyroidism.
- Almost one-third of women with hypothyroidism due to postpartum thyroiditis develop mild to moderate depression after pregnancy.
Problems In The Pituitary Gland
Hypothyroidism can also develop due to a problem in other parts of the thyroid hormone production line (namely the brain or pituitary gland). These cases of hypothyroidism, which do not originate in the thyroid gland, are much less common (perhaps 5%), and almost all of these cases are due to failure of the pituitary gland to produce or release the hormone TSH, which is responsible for stimulating the production of thyroid hormone in the thyroid gland. Diagnostic blood testing shows low levels of T3 and T4 thyroid hormones, low or absent TSH, and absence of the antithyroid antibodies characteristic of Hashimoto’s thyroiditis, the commonest cause of hypothyroidism.
Is Hypothyroidism Serious?
The presence and severity of symptoms are different for different persons. Although many symptoms of hypothyroidism cause distress, most are not dangerous themselves.
Indeed, proper diagnosis may be delayed or missed in older adults because the symptoms are considered “just part of getting old.” An individual may not seek help until tiredness, impaired memory, or other symptoms have affected daily living so much that a family member or friend asks them to see a doctor. Others may go to a doctor only when physical changes such as dry, flaking skin and facial puffiness have become obvious.
|
Need To Know: Untreated hypothyroidism can have serious consequences over the long term:
This need never occur with proper treatment. |
The good news is that treatment is simple, and the symptoms almost always resolve with treatment. Persons generally feel much better, more alert, and “back to being their old selves.”
The other major factor to consider in assessing how serious hypothyroidism is in any given individual is the presence (and, if so, severity) of associated health conditions.
How Is Hypothyroidism Diagnosed?
Diagnosis of hypothyroidism is based on a person’s medical history, a physical examination, and blood tests.
If a physician suspects hypothyroidism, he or she will look particularly at the cardiovascular system, the skin, hair, eyes, reflexes, and body temperature. The physical exam also may reveal an enlarged thyroid, which is called a goiter.
- In Hashimoto’s thyroiditis, if a goiter is present, it will not be tender and will have a rubbery feel.
- If the goiter is tender, the cause may be subacute thyroiditis, an inflammation of the thyroid that often follows an upper respiratory infection.
Blood tests check the levels of the thyroid hormones T4, T3, and TSH, among other related substances.
Abnormally low levels of T4 and T3 indicate hypothyroidism is present.
The TSH (thyroid-stimulating hormone) level is especially important in determining whether the condition is due to a problem in the thyroid gland or in the part of the brain that stimulates thyroid function.
- If the TSH level in the blood is high, the abnormality is within the thyroid gland. A high TSH level suggests that the thyroid gland is not responding properly to the stimulating effect of the TSH on the thyroid gland.
- If the TSH level in the blood is low, the abnormality is within the brain or pituitary gland in the brain. It suggests that the pituitary is not releasing adequate amounts of TSH to stimulate the thyroid gland, despite levels of thyroid hormone low enough that it should do so.
Among adults with hypothyroidism, roughly 95% of cases represent problems in the thyroid gland. In about 5% of cases, the abnormality is found in the brain or in the pituitary gland, almost always the pituitary gland.
If blood tests suggest that the problem is in the glands in the brain, imaging tests of the brain may be necessary. These include CT scans, which are sophisticated x-rays, and MRI scans, which use magnets to create images of the inner body.
Other blood tests include an antibody test, which is a blood test to detect antithyroid antibodies. High levels of these antibodies suggest that a person may have Hashimoto’s thyroiditis.
|
Need To Know: Of the blood tests for hypothyroidism, the TSH is the most sensitive test. The role of TSH is to stimulate the thyroid gland to produce thyroid hormone when the level of
|
|
Nice To Know: The American Thyroid Association, a national professional organization of thyroid specialists, recommends that women over age 35 should be screened every five years for hypothyroidism. |
How is Hypothyroidism Treated?
Treatment of hypothyroidism is simple. It involves taking daily thyroid hormone replacement medication. This supplies the body with thyroid hormone to replace what isn’t being produced by the thyroid gland.

The replacement thyroid hormone is artificially manufactured and is structurally identical to the thyroid hormone produced naturally in the body. It is a synthetic derivative of the thyroid hormone T4 and is calledlevothyroxine. Brand names include Synthroid, Levothroid, Levoxyl,Levo-T, as well as numerous generic preparations.
An adult typically starts with 0.1-0.15 milligrams per day, and the dosage is adjusted over time to reach normal blood levels, reflected by normal blood levels of TSH. It is important that older adults, especially those with heart disease, start at a low dose and increase it slowly. This minimizes the risk that the increase in metabolic activity due to thyroid hormone replacement therapy will stress the heart.
Because T4 is converted into
|
Need To Know: People differ in how quickly they respond to the medication. It is important to take the medication regularly as prescribed. Some hypothyroidism sufferers feel a marked improvement after only a couple weeks on medication. They find that their heart rate increases to normal range, they lose the weight they gained, and their skin and hair will return to normal. Some feel much improved in themselves only after a couple of weeks of treatment. It takes a little longer for the enlarged thyroid to decrease in size and for the “bad But others may find they still have various symptoms at six months or longer after beginning medication. If it’s taking that long, it’s usually because the dose is inadequate to bring the thyroid hormone levels into the normal range. The doctor may need to increase the dose, or perhaps try a combination of drugs with T4 and T3. A person who frequently forgets to take their medication will also not benefit from improvement in their symptoms.If the symptoms persist even though the blood tests of thyroid function are normal, it is likely that the symptoms are not due to thyroid hormone deficiency. |
It may be useful for an individual with newly diagnosed hypothyroidism to list their most distressing symptoms and to track changes in them over time after
Some people find that their physician will increase the dosage of their thyroid medication every year or two, in order to keep their blood levels of thyroid hormone within the normal range. This is because the inflammation of the thyroid gland may continue affecting more thyroid hormone producing cells, thus causing the thyroid to produce even less thyroid hormone than before.
|
Need To Know: It is important not to take too much thyroid hormone, since this can cause symptoms of For more information about hyperthyroidism, go to Hyperthyroidism. |
|
Nice To Know: Individuals diagnosed with subclinical hypothyroidism – when their TSH levels are high but thyroid hormone levels are normal, and they are not feeling any symptoms – are not always treated with replacement thyroid hormone. The decision is an individual one, made by the person and the physician. But up to half of such individuals will feel better after taking thyroid medication, and others will have improved cholesterol levels in the blood. |
For more information about treatment of hypothyroidism in infants, children, and teens, see What is the Treatment for Hypothyroidism in Infants and Children?
What Other Health Problems May Be Associated With Hypothyroidism?
Several potentially significant health conditions are common in persons with hypothyroidism. They include:

Goiter
Goiter is a general term for an enlarged thyroid gland that has the appearance of a swelling or fullness in the neck. Many persons with Hashimoto’s thyroiditis have a goiter. Although the thyroid gland is usually painless, there can be some discomfort. At the extreme, large goiters can interfere with swallowing, breathing, or both. In many cases, goiters decrease in size, often considerably, after thyroid hormone replacement therapy is begun. Surgery is rarely required.
|
Nice To Know: Before the connection of The cells of the thyroid gland increased in size and number in response to long-term high levels of TSH, the |
Heart Disease
One of the major organs affected by thyroid hormone is the heart. Increased heart rate and palpitations are common in persons with untreated
|
Need To Know: Persons who have hypothyroidism and heart disease should discuss their cardiac symptoms with their doctors before beginning thyroid hormone treatment.
|
High Cholesterol
The decreased metabolic activity associated with hypothyroidism leads to increased blood levels of cholesterol. Individuals whose blood cholesterol levels are found to be high, particularly if they do not have a previous history of high cholesterol, may be advised to have thyroid hormone levels checked. If the high cholesterol is due (at least in part) to hypothyroidism, improvement will come after hormone treatment is begun. A low-fat, low-cholesterol diet will also help; if cholesterol levels remain high, appropriate drug therapy may be needed to lower them.
Anemia
Anemia is the general term for any condition marked by a low red blood cell count. Because red blood cells carry oxygen between the lungs and the rest of the body, persons with anemia often feel tired with little exertion. This fatigue is in addition to the fatigue felt due to untreated hypothyroidism. Persons who have hypothyroidism, heart disease, and anemia become particularly tired and may develop angina or worsening of their angina.
Individuals with hypothyroidism may become anemic due to inadequate stimulation of red blood cell development in the bone marrow; this type of anemia (as well as persistent feelings of fatigue) usually goes away after thyroid hormone treatment is begun. Over-the-counter iron supplements and other preparations are not helpful.
However, if a premenopausal woman with untreated hypothyroidism has had heavy menstrual periods, she may have iron deficiency contributing to her anemic condition. These women will find iron supplementation useful in combination with their thyroid hormone treatment.
Hypothyroid persons with anemia, particularly elderly persons, should also be checked for possible
Infertility
Infertility is common in women whose thyroid hormone levels are low, and some women are diagnosed with hypothyroidism as part of a medical exam for infertility. After thyroid hormone treatment is begun, it is usually easier to conceive.
- Because thyroid hormone crosses the
placenta in small amounts, the thyroid hormone taken by the expectant mother may have important effects on the developing fetus. - Because the dose of thyroid hormone may need to be increased after a woman has conceived, it is valuable to get baseline (pre-pregnancy) thyroid tests (including TSH) and to periodically recheck during the pregnancy.
After delivery, the mother’s thyroid hormone needs typically return to pre-pregnancy levels.
If You Are Having Surgery
It is generally better to schedule elective surgery for one to two months after beginning
On the other hand, if there is a pressing need for surgery it usually can be performed safely in an untreated or partially treated person with hypothyroidism.
Hypothyroidism And Pregnancy
Hypothyroidism can develop during or after pregnancy. It also can affect a woman’s ability to become pregnant.

A woman has a 25% higher risk for developing hypothyroidism after pregnancy if she has diabetes or another autoimmune disorder. A miscarriage may be an indication that antithyroid antibodies were present before pregnancy. These antibodies do not cause the miscarriage, but seem to be a marker for other immune system problems that can lead to pregnancy loss.
How Hypothyroidism Can Affect Pregnancy
Hypothyroidism can affect pregnancy in several ways:
- It can cause infertility in women because it can prevent the production of eggs.
- A pregnant woman with hypothyroidism is at higher risk for miscarriage.
- Women with untreated hypothyroidism near the time of delivery are in danger of developing high blood pressure and premature delivery.
- Babies born to women with untreated hypothyroidism may not achieve their full intellectual potential.
Untreated hypothyroidism can cause serious problems for an unborn child, so many experts recommend that all pregnant women be tested for thyroid function during the pregnancy.
Every woman treated with thyroid hormone who anticipates becoming pregnant or is found to be pregnant should have her thyroid hormone levels monitored more closely. Some woman may need to have their dosage of medication increased by as much as 50% during pregnancy. Thyroid medication is safe to take during pregnancy.
A collaboration between a woman’s endocrinologist and obstetrician will maximize the chances for a successful pregnancy and delivery and make the mother’s postpartum adjustments as easy as possible.
Hypothyroidism Resulting From Pregnancy
One in every 20 women will develop hypothyroidism after pregnancy. This happens because they developed antibodies to their own thyroid prior to the pregnancy, and this caused an inflammation of the thyroid after delivery. This condition most often develops between four months to a year after delivery and usually resolves on its own. If it is long lasting or permanent, it is easily treated with medication.
|
Nice To Know: Q: We tried to conceive for several years, and now I’m finally pregnant. My obstetrician did some blood work when I went to see her, and she says I’m at risk for thyroid trouble after the baby comes. I don’t recall any doctor talking about my thyroid before. What does she mean? A: Postpartum thyroiditis (an inflammatory condition of the thyroid that develops after delivery) affects about 5% to 9% of mothers. About 80% to 90% of women who develop postpartum thyroiditis had antibodies directed against their |
Living With Hypothyroidism
Hypothyroidism can be treated easily and inexpensively with daily thyroid hormone (T4). This treatment supplies the hormone missing in the body and allows organs to return to a proper level of stimulation. Symptoms that had been distressing improve or disappear after hormone therapy has been begun.

Persons with hypothyroidism should remain aware of the symptoms of both hypothyroidism and hyperthyroidism so that they can alert their doctors if symptoms of either of these thyroid problems appear.
- Symptoms of hyperthyroidism occur when the body’s need for thyroid hormone decreases, and the previously correct dose becomes excessive. Changes that the individual might notice include a feeling of nervousness, a rapid heartbeat, intolerance of hot environments, and diarrhea.
- Symptoms of hypothyroidism occur when the body’s need for thyroid hormone increases, and the previously correct dose becomes inadequate. Changes that the individual might notice include feelings of physical and mental fatigue, a slowed heartbeat, intolerance of cold, and constipation.
Because thyroid hormone is simply a replacement for hormone no longer produced in the body, treatment does not require an individual to change lifestyle, give up alcohol, or make other changes. However, all individuals, regardless of gender or age, who take medications in addition to their thyroid hormone, should discuss the possibility of drug interactions with their doctors.
Some medications interfere with absorption of thyroid hormone from the digestive tract into the blood; such interference can keep the blood level of thyroid hormone low enough that symptoms of hypothyroidism continue or reappear. Two commonly used drugs that can interfere with thyroid hormone absorption are
- Cholestyramine, used for reduction of blood
cholesterol - Sucralfate, used in peptic ulcer disorders
If these drugs are required, they can be taken several hours apart from the thyroid hormone tablet. Also, iron and calcium supplements may interfere with thyroid hormone absorption. These too may be taken several hours apart from the thyroid hormone medication.
|
Nice To Know: Exercise is important to maintain health, but many people with hypothyroidism lack the energy to exercise. One expert suggests splitting exercise into several short sessions. |
Hypothyroidism: Frequently Asked Questions
Here are some frequently asked questions related to hypothyroidism.
Q: A neighbor of ours was recently diagnosed with hypothyroidism. She went to the doctor with the same kinds of problems I have: getting tired more easily, forgetting little things, feeling cold a lot of the time. Now, my granddaughter thinks I should go, too. I don’t feel sick, I’m just getting older. What should I do?
A: It makes sense to ask your doctor if you might have hypothyroidism. The testing is simple: just a sample of blood from your arm. The treatment is simple: a daily dose of
Q: I was confused when I asked my doctor about my thyroid hormone level and she talked about
A: Two slightly different forms of thyroid hormone are found in the blood. One is abbreviated as T3 (thyroid
Q: The doctor said my hypothyroidism isn’t due to a problem in my thyroid gland, but instead something wrong in another gland, one in my head. Does that make sense?
A: Although the vast majority of cases of hypothyroidism result from a problem in the thyroid gland, up to about 5% of cases are due to a problem in the
Q: My sister’s doctor retired, and she went to a new one. He did some tests and told her she has hypothyroidism from a condition called
A: There is a genetic factor in developing Hashimoto’s thyroiditis, and there is often a familial tendency toward it and other autoimmune disorders. Because Hashimoto’s thyroiditis is more common in older women, both you and your sister might be at higher risk for developing it, particularly if there is a positive family history (as there might be if your aunt was affected, too). Discuss it with your doctor.
Q: We tried to conceive for several years, and now I’m finally pregnant. My obstetrician did some blood work when I went to see her, and she says I’m at risk for thyroid trouble after the baby comes. I don’t recall any doctor talking about my thyroid before. What does she mean?
A:
Q: My husband had bypass surgery three years ago. He was recently diagnosed with hypothyroidism, and the doctor asked him a number of questions about how he was feeling, if he was having any attacks of angina, getting short of breath on stairs, etc. Is his hypothyroidism making his heart disease worse?
A: Actually, the decreased metabolic activity associated with hypothyroidism decreases the workload on the heart. Your husband’s doctor may have been concerned because the increased metabolic activity associated with starting thyroid hormone treatment will increase the workload on the heart somewhat. The best thing for your husband to do is talk with his doctor about how he feels, any concerns he has about possible strain on his heart while starting thyroid hormone treatment, and what steps can be taken to minimize stress on his heart.
Q: I’ve gotten routine physicals for years, and my blood work was always fine. Now my
A: The decreased metabolic activity associated with hypothyroidism leads to an increase in blood cholesterol levels. Because you haven’t had high cholesterol in the past, your doctor may feel your current cholesterol level represents undiagnosed hypothyroidism. A simple blood test can check your thyroid gland function. If you have hypothyroidism, a daily dose of thyroid hormone will correct your hormone level, restore proper body metabolic activity, and bring your cholesterol level back to its previous, normal level.
Hypothyroidism: Putting It All Together
Here is a summary of the important facts and information related to hypothyroidism.
- Hypothyroidism is the condition marked by too little
thyroid hormone in the blood. - Symptoms of hypothyroidism include slowed heartbeat, tiredness, difficulty thinking and remembering, dry and flaky skin, constipation, and inability to tolerate the cold.
- Hypothyroidism can occur at any age, from birth well into the senior years.
- Diagnosis of often delayed or missed because symptoms are subtle and can be attributed to other causes, such as aging or stress.
- Hypothyroidism is diagnosed with a medical exam and blood testing.
- The condition can be easily and successfully treated with medication that replaces the thyroid hormone that is lacking in the body.
- Regular monitoring via blood testing provides the means for ensuring appropriate
hormone replacement therapy for the rest of one’s life. - Hypothyroidism can affect a woman’s ability to become pregnant and also the health of her unborn child. Pregnant women can safely take thyroid medication, as it does not affect a developing fetus adversely.
- Most of the symptoms of hypothyroidism improve greatly or disappear after thyroid hormone treatment is begun.
- Thyroid hormone treatment may be needed for life, but fortunately treatment is simple, inexpensive, and easily monitored.
Hypothyroidism: Glossary
Here are definitions of medical terms related to hypothyroidism.
Adam’s apple: This part of the cartilage that forms the larynx, or voice box, can be felt at the front of the neck. It is more prominent visually and by touch in men than in women.
Anemia: Any condition characterized by a low red blood cell count. A low red blood cell count decreases the body’s ability to use oxygen, and thus, to work. Anemia is associated with easy fatiguing, even with mild exertion.
Angina (or angina pectoris): A sudden pain that can be felt in the chest, lower jaw, or down the left arm that is due to insufficient blood flow to heart muscle, usually due to narrowing of the coronary arteries, the arteries that supply the heart muscle with blood.
Antibody: A protein made by the body’s immune system to defend the body against a foreign substance like a virus, bacterium or other foreign body, most often a foreign protein. Rarely, the body’s immune system may mistakenly make antibodies against itself. This is an abnormal or autoimmune response.
Antithyroid drug: Any one of several agents used to treat hyperthyroidism that decreases production of thyroid hormone within the thyroid gland.
Autoimmune disorder: An autoimmune disorder is one in which the body’s immune system mistakenly “attacks” its own healthy tissue.
Cholesterol: A fatty substance found naturally in animal cells, including human cells. High levels of cholesterol in the blood are correlated with arteriosclerosis, the condition marked by deposits of fatty materials inside blood vessels leading to their narrowing or obstruction.
Endocrine gland: A gland that releases a chemical messenger, known as a hormone, directly into the bloodstream, that will affect other parts of the body. The thyroid is an endocrine gland.
Endocrinology: The subspecialty within internal medicine devoted to disorders of the endocrine glands. The specialist is called an endocrinologist.
Goiter: An enlarged thyroid gland due to any cause. It is seen as a swelling or fullness in the front of the neck.
Graves’ disease: An autoimmune disorder in which the immune system attacks the cells of the thyroid gland causing hyperthyroidism. Hyperthyroid eye changes and skin changes are sometimes associated with it.
Hashimoto’s thyroiditis: An autoimmune disorder of the thyroid gland in which the body’s immune system attacks the thyroid gland, destroying the cells of the thyroid gland
Hormone: A chemical substance that is produced by an endocrine gland and released into the bloodstream to have its effect on other parts of the body. Also known as a “chemical messenger”. For example, thyroid hormone, released by the thyroid gland speeds up or stimulates certain bodily functions.
Hyperthyroidism: A condition in which too much thyroid hormone is circulating throughout the body, causing excessive stimulation of metabolic activity in body cells.
Hypothyroidism: A condition in which too little thyroid hormone is circulating throughout the body, causing inadequate stimulation of metabolic activity in body cells.
Immune system: The body system (consisting primarily of white blood cells) that enables the body to fight infection and defend itself against foreign invaders.
Infertility: Inability to become pregnant.
Iodine: A chemical element found naturally in seawater and some other sources that is needed to produce thyroid hormone. Iodized table salt has had iodine added to it.
Juvenile diabetes mellitus: Also known as insulin-dependent diabetes, this form of the disease most commonly develops in children and young adults.
Metabolism: The chemical and physical processes in the body that create the substances and generate the energy needed for cells to function, grow normally, and divide. Metabolism is also known as metabolic activity.
Pernicious anemia: A form of anemia, which means less than the normal level of circulating red blood cells. This condition is caused by an inappropriate autoimmune process in which the immune system attacks and damages certain cells lining the stomach. As a result, vitamin B12 is not absorbed properly from food that is consumed. Vitamin B12 is necessary for proper red blood cell production.
Pituitary gland: A relatively small endocrine gland about the size of a pea. This gland is located underneath the brain and releases a number of essential hormones, including thyroid stimulating hormone (TSH).
Placenta: The structure within the pregnant uterus that is the interface between the maternal and fetal bloodstreams. Oxygen, food substances, and other materials pass from the mother’s bloodstream to the fetus’s through the placenta. Many drugs cross the placenta to enter the fetal bloodstream.
Postpartum thyroiditis: Inflammatory condition of the thyroid probably of autoimmune origin. It occurs in 5%-9% of women following childbirth. Although the hypothyroidism associated with it is usually temporary, it can become permanent in up to one third of affected women.
Radioactive iodine: Chemically depicted as 131I, this form of iodine is radioactive, which means it emits intense energy due to chemical reactions in the nucleus. It is often used in the treatment of hyperthyroidism.
Subacute thyroiditis: Inflammatory condition of the thyroid of unclear origin, it often follows an upper respiratory infection. The hyperthyroidism and hypothyroidism associated with it is usually mild and temporary.
Synthetic thyroid hormone: Thyroid hormone (T4) that is artificially manufactured but is structurally identical to that naturally produced in the body.
T3: A term used to describe a form of thyroid hormone in the bloodstream. It has three units of iodine attached to the hormone structure. T3 is biologically active.
T4: A term used to describe a form of thyroid hormone in the bloodstream. This form has four iodine units attached to the hormone structure. Most thyroid hormone in the blood is T4; however, it is not biologically active in the body. Special cells convert T4 into T3.
Thyroid gland: Small, butterfly-shaped organ located in the neck below and in front of the Adam’s apple, which produces thyroid hormone.
Thyroid hormone: Chemical substance produced by the thyroid gland and released into the bloodstream. It interacts with almost all body cells, causing them to increase their metabolic activity. Two forms of thyroid hormone, abbreviated as T3 and T4, are found in blood.
Thyroid-stimulating hormone (TSH): Hormone produced by the pituitary gland that interacts with thyroid cells causing them to produce and release more thyroid hormone into the blood.
Vitamin B12: A chemical substance found almost exclusively in meats that is necessary for certain chemical processes in the body, including the ongoing production of red blood cells.
Vitiligo: An autoimmune skin disorder caused by attack of the immune system on the pigment-producing cells within the skin. The loss of the cells responsible for skin color result in milky white patches on the skin surface.
Hypothyroidism Additional Sources Of Information
Here are some reliable sources that can provide more information on hypothyroidism.
A number of organizations offer information, support, and advocacy for persons with thyroid diseases including
Thyroid Foundation of America (TFA)
Phone: 800-832-8321
www.tsh.org
This organization provides contact information for a number of national organizations. Information in French is available through the TFC site.
American Thyroid Association
http://www.thyroid.org
Healthfinder, an Internet health information service developed in conjunction with the US Department of Health and Human Services.
http://www.healthfinder.gov
This site offers information in Spanish.
