In this Article
Deep Vein Thrombosis
What Is Deep Vein Thrombosis (DVT)?
Deep vein thrombosis (DVT) is a condition in which blood clots form in a vein deep within the body. The word thrombosis means forming a blood clot. The clot itself is called a thrombus.

A blood clot is a jelly-like mass of congealed blood. Clotting is the normal way the body stops bleeding and begins healing following injury. Once the clot has done its job, the body absorbs it. Sometimes, however, blood clotting can prove harmful.

DVT occurs when a blood clot forms in a deep vein and remains there.
DVT usually involves the formation of a large clot in the deep veins in the lower legs and thighs. In rare instances, DVT can occur in the area around the armpit and collar bone (axillary-subclavian vein thrombosis), in the upper arm, abdomen, or pelvic region.
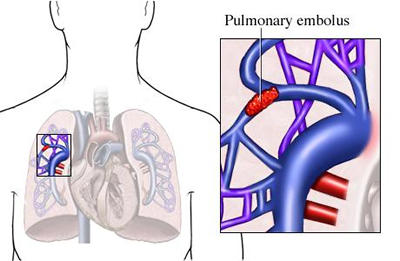
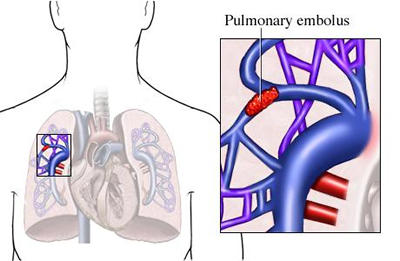
It is a dangerous condition because the clot may become dislodged from the vein and travel inside the vein all the way to the lung, where it may get trapped and block a vessel in the lung. This is called pulmonary embolism, which can be deadly.
Deep vein thrombosis most often occurs in:
- Hospitalized patients following surgery.
- Individuals confined to bed for prolonged periods.
- Healthy individuals whose legs remain immobilized for long stretches of time, such as passengers on lengthy airline flights.
| Need To Know:
Because deep vein thrombosis can have serious consequences, early detection is essential to prevent complications like pulmonary embolism. Surgeons, for example, are always on the lookout for DVT following surgery. |
| Need To Know:
Q. Who is at risk for deep vein thrombosis? A. Some people are more likely than others to develop thrombosis. Those at risk include:
|
Facts about deep vein thrombosis:
|
What Causes Deep Vein Thrombosis?
Veins are thin-walled blood vessels that carry blood from the body tissues back to the heart. In order to move the blood from the legs toward the heart, the leg muscles squeeze the deep veins, forcing the blood upward.

Deep vein thrombosis is the result of three principal factors (described by Dr. Virchow in the 1860′;s):
- Reduced or stagnant blood flow in deep veins (venous stasis).
- Injury to the blood vessel wall.
- An increase in the activity of those substances in the blood that are part of the normal clotting mechanism, a condition called hypercoagulability (which means a more active clotting state).
A number of factors can bring about these conditions, thus increasing the possibility of developing DVT. These include:
- Immobilization, such as lying in bed following surgery
- Having undergone a surgical procedure
- Having been subjected to major trauma
- Increasing age
- Malignancy (cancerous tumor)
- Heart failure
- A previous bout with deep vein thrombosis
- Pregnancy
- The use of oral contraceptives
|
Need To Know: Surgical procedures that are most often associated with deep vein thrombosis are:
|
The following factors also put people at greater risk of developing a blood clot:
- Prolonged immobilization (such as on a long car or airplane trip) – sitting for long periods (4 hours or more) reduces circulation in legs by 50 percent.
- Diabetes (a disorder in which the body can not make use of sugars and starches in a normal way), which damages blood vessels.
- Obesity – weight puts pressure on veins, causing them to weaken.
- Childbirth – physical strain of childbirth puts pressure on deep veins, causing them to weaken.
- Tobacco smoking – damages blood vessels and doubles the risk of thrombosis.
Signs And Symptoms of Deep Vein Thrombosis (DVT)
Only 40 to 50 percent of people with DVT have obvious signs and symptoms of DVT, and the condition often goes unrecognized.
When they do occur, signs and symptoms vary depending on the severity of the condition.
DVT may cause pain and swelling in one or both legs, or less commonly, in an arm. There may also be tenderness in the affected area, and an increase in skin temperature (compared to the unaffected limb).
Signs and symptoms of deep vein thrombosis include:
- Pain in the leg
- Tenderness in the calf (this is one of the most important signs)
- Leg tenderness
- Swelling of the leg
- Increased warmth of the leg
- Redness in the leg
- Bluish skin discoloration
- Discomfort when the foot is pulled upward
With DVT high up in the leg (ileofemoral vein), superficial veins may become visible over the thigh and hip areas as well as over the lower abdomen.
|
Nice To Know: Swelling in one leg following childbirth was, for centuries, called “milk leg,” because the swelling was believed to be caused by milk retained by mothers who did not nurse. Others thought it was due to infection or the blockage of lymph nodes. Eventually, investigations performed in the early part of the 1800s showed that the swelling was due to thrombosis in deep veins of the thigh. Today, this type of deep vein thrombosis following pregnancy, in which the painfully swollen leg appears pale in color, is called phlegmasia alba dolens. |
Conditions That May Cause Similar Symptoms
There are a number of different conditions that can cause signs and symptoms similar to deep vein thrombosis. These include:
- Muscle aches and tears
Superficial thrombophlebitis – a blood clot that forms in an inflamed part of a vein near the surface of the body (i.e., not a deep vein)- Varicose veins – blood vessels that are abnormally swollen and twisted
- Blood clots in arteries
- Arthritis
Cellulitis – an infection in tissue under the skin- Bone fracture
Lymphedema – swelling in the hands and feet caused by excess fluid retention
How Is Deep Vein Thrombosis Diagnosed?
The diagnosis of deep vein thrombosis is suspected on the basis of signs and symptoms alone. An examination may reveal a red, swollen, tender area of the leg, particularly the calf. A sharp pain when the foot is flexed upward sometimes suggests that the individual has DVT.
|
Need To Know: The importance of correct diagnosis If a diagnosis of DVT is strongly suspected, physicians may start treatment with anticoagulant (blood-thinning) drugs before tests have confirmed the diagnosis. These drugs, however, can lead to internal bleeding. Therefore, physicians are reluctant to start treatment until tests have definitively diagnosed the condition. |
For a definitive diagnosis of DVT, special imaging techniques are required.
- Ultrasound, a diagnostic technique which uses harmless high frequency sound waves to measure blood flow in the deep veins.
In this procedure, a detector is passed over the skin of the affected limb. Sound waves painlessly penetrate the skin, bounce back from the structures below, and are converted to electrical impulses. After processing, these impulses form an image of the tissues inside the leg on a monitor. Blood flowing through an obstructed vein creates a different image than blood flowing through a fully open vein.
- Venography. Until recent advances in ultrasound made the procedure highly reliable, the best method for diagnosing deep vein thrombosis was venography, which is still used. It remains the “gold standard” for definitive diagnosis.
Venography uses X-ray technology to measure blood flow in deep veins. A special harmless dye is injected into a vein in the foot. This substance then circulates throughout the veins in the leg and can be easily seen on an X-ray. If DVT is present, blockages or partial blockages in the vein are immediately seen; the dye is seen surrounding any clot that exists in the vein.
- Blood test coagulability (clotting tendency). Various tests are used to assess the activity of the blood clotting factors. The time taken for the person’s blood to clot is measured and compared with the time taken for normal blood to clot under the same conditions.
- Other tests. Rarely, physicians will use computerized tomography scanner or CT scan (a machine that passes X-rays through the body from various angles) to diagnose DVT in the abdomen or pelvic region. In some instances, they will usemagnetic resonance imaging (MRI) . Both techniques provide high quality cross-sectional images of organs and structures within the body.
- If a pulmonary embolism is suspected, specialized tests will be immediately ordered. These include a lung perfusion scan or a pulmonary arteriogram, in which dye is injected into an artery and its course followed through the lungs. Any obstruction due to a clot will be seen. A perfusion scan determines if there is an area of the lung not being properly ventilated. Specialized blood tests and an EKG will also be done.
Complications of Deep Vein Thrombosis
Fortunately, most cases of deep vein thrombosis improve with treatment. However, DVT can result in serious complications.
Pulmonary embolism
Chronic venous insufficency
Pulmonary Embolism
The most serious complication of DVT occurs when a clot becomes dislodged from a vein, travels to the lung, and blocks or partially blocks the pulmonary artery leading from the heart to the lungs. This condition is called pulmonary embolism.

If the clot is small, only one or more portions of the lung may be deprived of blood and damaged. This condition can result in:
- Shortness of breath
- Chest pain with breathing
- Bloody sputum (material coughed up from the lungs)
If a blood clot blocks the pulmonary artery, pulmonary embolism can be fatal due to the inability of blood to circulate through the lungs.
Vigorous treatment is immediately begun with blood-thinning drugs, oxygen and other medications depending on the situation.
Multiple and repeated emboli can lead to chronic impairment of blood circulation through the lungs and cause a form of heart failure.

Long-term DVT can degenerate the valves in veins that control blood flow.
This may result in swelling of the leg and ankle and skin disorders, such as dermatitis (inflammation of the skin) and
|
If you know you have DVT or have had a recent surgery, go to the emergency room immediately if you experience chest pain, difficulty breathing, fainting, loss of consciousness, or other severe symptoms. |
|
Q. Can DVT lead to amputation? A. Most cases of amputation associated with blood clots involve clots of the arteries. Such clots prevent the flow of blood to tissues beyond the blockage, causing tissue death (necrosis). Rare instances of amputation associated with deep vein thrombosis occur in individuals with “blue leg” (phlegmasia cerulea dolens), in which there is a massive venous thrombosis of the upper leg as well as an advanced malignancy (cancer) elsewhere in the body. |
How Is Deep Vein Thrombosis Treated?
Treatment of DVT is aimed at:
- Easing symptoms
- Preventing worsening of the clot
- Preventing the clot from traveling to the lungs
Treatment usually requires hospitalization, primarily to facilitate monitoring of medications. Because DVT occurs in post-surgical patients, however, the person might already be in the hospital when DVT is diagnosed.
Deep vein thrombosis must be treated promptly. Once the diagnosis is confirmed, the individual is kept in bed with the foot of the bed elevated.
- Bed rest. Individuals with DVT usually require bed rest until symptoms are relieved. The leg should be elevated to a position above the heart to reduce swelling (the foot of the bed is elevated about six inches to achieve this). Moist heat may be applied to the affected region to relieve pain.
- Compression stockings. Physicians frequently recommend that people who have DVT wear compression stockings (also called support hose) to reduce symptoms. Compression stockings improve circulation by providing a graduated pressure on the leg to help return the venous blood to the heart.
- Blood-thinning drugs. Treatment with anticoagulants (commonly known as blood thinners) is required in most cases of DVT. The anticoagulant drugs heparin and warfarin are used primarily to prevent the formation of new clots, and, thus, reduce the chance of pulmonary embolism.
- Heparin is the anticoagulant drug of first choice. It must be administered intravenously (an injection made directly into a vein).
- Warfarin (also called coumarin) is taken by mouth.
- Treatment with heparin normally lasts seven to 14 days. Treatment with warfarin is usually continued from two to six months, depending on the age of the person, the severity of the DVT, and whether risk factors are present.
- Clot-busting medication. Drugs called thrombolytic agents (clot-dissolving medications) are used to help dissolve existing clots and reopen clogged veins. The most commonly used thrombolytic agents are urokinase, streptokinase, and recombinant tissue plasminogen activator (rt-PA).
Need To Know:
Anticoagulants (blood-thinning medications) can cause internal or external bleeding as a result of the blood being diluted to prevent unnecessary clotting. People taking anticoagulants require regular blood tests to ensure that the correct dosage is maintained.
The dosage of the blood-thinning drugs is adjusted as appropriate to achieve an INR between two and three. The INR is a test that compares how long it takes the patient’s blood to clot while on blood thinners, against normal clotting times.
A person on anticoagulant medication should carry a card naming the anticoagulant drug and stating the dosage.
The best results occur when this treatment is given to people who have had DVT for less than 48 hours.
When effective, the clot usually breaks up within 24 to 48 hours.
Thrombolytic agents can also cause internal and external bleeding, and require careful monitoring. Treatment with thrombolytic agents usually lasts for only 24 to 72 hours.
- Surgery. If an
embolus develops, surgery may be necessary to prevent the spread of the clot to the lung. Surgery, however, is performed only as a last resort.Surgery for complications resulting from DVT involves the insertion of a filter into a large blood vessel to trap any blood clots headed toward the lungs. The filter allows blood to flow through it normally, but traps the traveling clots. The procedure is called vena cava interruption because the filter is placed in the inferior vena cava, the large vein in the pelvic area that receives the blood returning from the deep femoral (thigh) veins.

The most severe cases of DVT may require the surgical removal of the blood clot from the vein, a procedure known as venous thrombectomy. The patient is given anticoagulant therapy with heparin during the surgery, and warfarin for a period of at least six weeks to three months following the operation.
Preventing Deep Vein Thrombosis
Because of the potential serious consequences of DVT, prevention is essential. The possibility of DVT is on every surgeon’s mind, and surgeons aim aggressively to prevent it.
Thus, doctors urge patients who have undergone surgery to get out of bed and walk as soon as possible. Also, post-surgical patients are asked to wear anti-embolism stockings (lightweight, stretchy hose that cover the leg from the toes to the top of the thigh) while lying in bed.
Other measures include:
- Low-dose,
intravenous (an injection made directly into a vein) heparin therapy beginning just before a major surgical procedure and continuing for a few days thereafter, particularly for those at risk. Heparin is a drug that helps prevent blood clotting. - Intermittent pneumatic leg compression. This procedure uses an inflated cuff to squeeze the muscles in the affected leg. The action helps improve blood flow in deep veins.
- Low-dose oral anticoagulant therapy. Aspirin and/or the blood-thinning drug warfarin are typically used in this treatment.
- Intravenous administration of a modified form of heparin (low molecular weight heparin). This treatment is especially useful in patients who have undergone elective hip and/or knee surgery.
Compression stocking . Patients are usually advised to put the stockings on before they get out of bed and to wear them all day.
Deep Vein Thrombosis: Frequently asked questions
Here are some frequently asked questions related to deep vein thrombosis.
Q: Didn’t I read somewhere that poison extracted from certain snakes was being used in thrombolytic therapy?
A: Although certain snake venoms have been studied for their blood-thinning properties, they are not useful in treating deep vein thrombosis.
Q: Can DVT lead to amputation?
A: Most cases of amputation associated with blood clots involve clots of the arteries. Such clots prevent the flow of blood to tissues beyond the blockage, causing tissue death (necrosis). Rare instances of amputation associated with deep vein thrombosis occur in individuals with “blue leg” (phlegmasia cerulea dolens), in which there is a massive venous thrombosis of the upper leg as well as an advanced malignancy (cancer) elsewhere in the body.
Q: How likely is it that a thrombosis will cause pulmonary embolism?
A:
Deep Vein Thrombosis: Putting It All Together
Here is a summary of the important facts and information related to deep vein thrombosis.
- Deep vein thrombosis is a condition in which blood clots form in deep veins of the body, most commonly in a leg.
- Deep vein thrombosis is a fairly common problem, especially among hospitalized patients who have undergone major surgery, and in other individuals requiring prolonged bed rest.
- The condition can lead to blockages of blood vessels in the lungs, which can be life-threatening.
- Measures can be taken to prevent or minimize the possibility of deep vein thrombosis following major surgery.
- Most cases of deep vein thrombosis can be successfully treated with medication.
Deep Vein Thrombosis: Glossary
Here are definitions of medical terms related to deep vein thrombosis.
Cellulitis: An infection in tissue under the skin.
Compression stocking: A tightly fitted sock, either from the toes to the knee or to the top of the leg, which applies a gentle pressure to the leg and helps with the flow of blood in the veins.
Computerized axial tomography scanner (CT scan): A noninvasive imaging technique that passes X-rays through a patient’s body from various angles.
EKG (electrocardiogram): A test to record the electric currents produced by the heart.
Embolus: A blood clot that detaches from the inside of a blood vessel and travels in the bloodstream (can also be fat, air, or a piece of tumor).
Iliofemoral vein: A large vein located in the groin area.
Intravenous: An injection made directly into the vein.
Lymphedema: Swelling in the hands and feet caused by blockage of the lymphatic transport system.
Magnetic resonance imaging (MRI): An imaging technique that uses powerful magnets to create very clear images of the inside of the body.
Post-partum: The period following a live birth.
Superficial thrombophlebitis: A blood clot that forms in an inflamed part of a vein near the surface of the body.
Thrombus: A blood clot.
Ulcers: Open sores; a break in the skin.
Varicose vein: A vein that is abnormally widened and twisted due to defective valves in the vein.
Deep Vein Thrombosis: Additional Sources of Information
Here are some reliable sources that can provide more information on deep vein thrombosis.
National Heart Lung and Blood Institute
http://www.nhlbi.nih.gov/
