In this Article
Palpitations
What Are Palpitations?
Palpitations are the awareness that your heart is beating forcefully, rapidly, or irregularly. There often is a feeling of “skipping beats” or “fluttering in the chest.” They can occur in normal healthy people, as well as in people with heart problems.
Palpitations can be very frightening. But most palpitations do not indicate underlying heart disease. If you are having palpitations, there is a good chance that nothing is seriously wrong.
Normally, people do not notice their hearts beating. But palpitations are common in everyday life and can happen to anybody, regardless of whether the person has an underlying heart abnormality.
Usually, palpitations do not last long. They are more likely to happen as you get older, although young people can have them too. Often, the cause of palpitations cannot be determined.
A variety of painless tests are available to help your doctor determine whether or not you need medical treatment.
|
Nice To Know: Irregularities of the heartbeat were recognized as early as the 1870s. Some years later, a German doctor invented the electrocardiograph, a device that records the electrical activity of the heart. With this tool, physicians determined that extra electrical impulses were the cause of extra heartbeats. James Mackenzie (1848-1924) was a Scottish cardiologist who was first to identify the large number of irregularities in the heart’s beating action. He established which irregularities were caused by serious disease and which were of no consequence. He is considered to be a pioneer of modern cardiac medicine. |
|
Nice To Know: Q: Every once in a while, I could swear that my heart actually skips a beat. Can this be harmful in the long run? A: A feeling of skipped heartbeats is a very common description of palpitations. In most cases, it has nothing to do with how well your heart is performing. You are especially likely to notice skipped heartbeats if you are tired or have had too much caffeine or alcohol. |
Understanding How The Heart Works
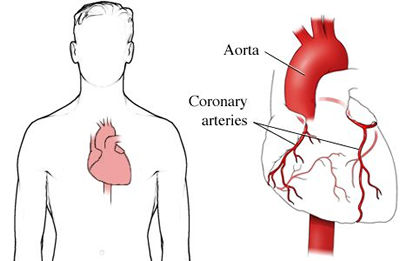
The heart is a muscle. It has four chambers: two upper ones, called the atria, and two lower ones, called the ventricles. Blood flows in and out of the heart through these chambers.
The Heart As A Pump
The heart pumps blood to the lungs to absorb the oxygen we inhale. It then pumps this oxygen-rich blood to the rest of the body through the arteries. After the blood delivers the oxygen to the body’s tissues, it returns to the heart through the veins. The cycle is then repeated.
Here’s how the pumping system works:
- Oxygen-poor blood returns from the body to the right upper chamber of the heart, called the right atrium. This chamber contracts to pump the blood to the right ventricle.
- The right ventricle pumps the blood into the lungs, where it takes up oxygen and gets rid of carbon dioxide.
- Next, the oxygen-enriched blood travels to the left atrium, which pumps it into the left ventricle.
- The left ventricle then pumps the blood to tissues throughout the body via the arteries.

What Makes The Heart Beat?
Heartbeats – the contractions of the heart muscle – are controlled by electrical signals. These signals are low-voltage signals that are normally generated in an area of the heart called the
Here’s how the heart’s electrical system, also called the conduction system, works:
- The sinus node, also called the sinoatrial (SA) node, lies in the wall of the right atrium (the upper right chamber of the heart). Electrical impulses generated here are spread to both atria and cause them to contract (pump).
- Special pathways carry impulses from the sinus node to the atrioventricular (AV) node. The role of the AV node is to momentarily delay the impulse to allow the atria to complete their contraction before the ventricles contract. This helps the ventricles fill with blood, especially at fast heart rates.
- From the bottom of the AV node emerges the atrioventricular bundle. This cable-like structure – the only normal route for conduction of impulses from the atria to the ventricles – splits into two pathways, called the right and left bundle branches.
- The bundle branches divide into fibers that spread electrical impulses throughout the ventricles. The high speed at which impulses travel through these fibers ensures that both ventricles contract almost simultaneously, increasing the effectiveness of contraction and pumping of blood.
How Is The Heartbeat Regulated?
The ability of the heart to contract is a property of the heart muscle itself; it is not dependent on the body’s nervous system. So even if nerve connections to the heart are cut, the heart continues to contract, as demonstrated by transplanted hearts.
However, the heart is well supplied by nerve fibers, and these can affect the basic activity of the heart. Other factors that determine the heart’s rate (the number of beats per minute) and rhythm (the sequence of heartbeats) include:
- Chemical messengers
- Age
- Body temperature
- Levels of electrolytes (salts) in the blood
Normally, the sinus node sets the pace of the heart. At rest, the sinus node usually fires between 60 and 100 impulses per minute, and the associated rhythm is called sinus rhythm.
But under certain conditions (for example, exercise, stress, decreased blood volume, low blood pressure), the sinus node speeds up the rate at which it generates impulses. This happens in order to speed up the heart rate to provide the increased blood supply that the body needs.
The message to the sinus node to speed up is sent by the nervous system and by chemical messengers called
What Other Factors Influence The Heartbeat?
A variety of other factors also influence the heartbeat:
- Certain medications
- Lifestyle factors (for example, stress or the use of nicotine, caffeine, or alcohol)
- Diseases
Irregularities in the normal rate and rhythm of the heart are called arrhythmias. Examples of arrhythmias are:
- A fast heartbeat, called
tachycardia - A slow heartbeat, called
bradycardia - An irregular heartbeat
Symptoms of an
- A skipping or fluttering sensation in the chest (palpitations)
- Light-headedness
- Fainting
- Chest pain
- Shortness of breath
|
Nice To Know: Not everyone experiences symptoms, however. In some people, arrhythmias may go unnoticed. |
Arrhythmias may occur if the sinus node develops an abnormal rate. In other cases, arrhythmias may mean that another region of the heart (such as the AV node or ventricle) has assumed the role of cardiac pacemaker.
Under normal conditions, these other regions do not control the heartbeat, as they fire impulses at slower rates than the sinus node. However, any of these regions may assume the role of pacemaker if the sinus node fails or if its impulses are blocked or interrupted. In addition, various diseases (including heart disease), drugs, and nervous system stimulation may contribute to this condition.
What Causes Palpitations?
Palpitations usually occur when something disrupts the normal electrical activity or function of the heart. They may be felt when the heart is beating quickly, slowly, or irregularly (an arrhythmia) or when the heart is contracting more forcefully than usual. Sometimes, palpitations occur for unknown reasons in people with no evidence of heart disease or arrhythmias.
Arrhythmias may occur in otherwise healthy individuals in response to lifestyle factors, prescription medications, or other drugs. In some individuals, arrhythmias occur due to an underlying condition or illness.
Lifestyle factors that can cause palpitations include:
- Strong emotions
- Strenuous exercise
- Smoking
- Consuming too much of a caffeinated beverage (such as coffee, tea, cola) or other caffeine-containing product (such as chocolate)
- Drinking too much alcohol
- Stress or anxiety
- Certain medications (such as diet pills or thyroid hormone replacement)
- Certain over-the-counter medications (such as decongestants), certain diet supplements, and “recreational” drugs
Conditions that can cause palpitations include:
- Serious illness or fever (which can increase the heart rate)
- Nausea and vomiting (which can affect the nervous system and slow the heart rate)
- Thyroid gland disease
- Anemia (a condition in which your number of red blood cells is less than normal)
- Heart disease
- Lung disease
- Adrenal gland tumor
- Hypoglycemia (low blood sugar)
When Are Palpitations Serious?
Palpitations can be very frightening. But most palpitations do not indicate underlying heart disease. If you are having palpitations, there is a good chance that nothing is seriously wrong. See What are palpitations.
So when are palpitations serious?
Palpitations could be a reason for concern if they are caused by an underlying heart disorder (such as heart valve disease or coronary artery disease) or another serious condition. In this case, they may occur more frequently or may continue for a prolonged period of time. They can happen unexpectedly or might occur after only a modest amount of physical activity.
Your palpitations might be serious if they are accompanied by other symptoms, such as:
- Sweating
- Faintness
- Chest pain
- Shortness of breath
- Dizziness
- Loss of consciousness
These symptoms can be signs of a serious disturbance in the heart’s rhythm and, perhaps, underlying heart disease. However, it is not easy to tell the difference between palpitations that occur in healthy individuals and those that are linked to heart disease. Your doctor can make that diagnosis.
Changing Heartbeat And Palpitations
Palpitations may occur with changes in the:
- Heart rate, which is the speed at which the heart beats
- Heart rhythm, which is the pattern of the heart beats
- Force of ventricular contraction, which reflects how vigorously the heart is pumping
Arrhythmia is the term used to describe irregularities or abnormal patterns of the heart’s pumping cycle.
Arrhythmias (irregular heartbeats):
- May be present for just a few beats at a time – this creates palpitations experienced as an extra or skipped heartbeat
- May last for longer periods in the form of a fast heart rate (tachycardia)
- May involve slow heart rate (bradycardia).
Palpitations Associated With Extra Heartbeats
Premature heartbeats (contractions) are beats that occur earlier than expected, briefly interrupting the normal heart rhythm. They are the most common abnormality of the heart rhythm and are often experienced as a “thump” in the chest or a missed beat.
This sensation does not reflect the premature beats themselves, but rather the forceful beat that follows the pause after the premature beat. The heart has more time to fill with blood during this pause, making the next beat more forceful.
|
Nice To Know: Ask the Doctor Premature beats may originate from anywhere in the heart. If you are experiencing extra heartbeats, you may want to ask your doctor what type of premature beat you have. This can help you understand the possible causes and treatment, if necessary. Type of premature beats are:
|
Extra heartbeats occur frequently in healthy individuals as well as in those with underlying heart disease. Many people report extra beats when they are exhausted or after having too much alcohol or caffeine. In most cases, premature contractions are not serious and do not require treatment. However, if PVCs are frequent or occur in certain patterns, they may be a sign of a more serious problem.
Palpitations Associated With A Fast Heart Rate
A fast heart rate of greater than 100 beats per minute is known as tachycardia (from the Greek adjective for swift).
Tachycardias can be an appropriate response to exercise or other causes (such as fever, blood loss, or low blood pressure). Other tachycardias may reflect underlying heart disease, problems with the electrical system of the heart, or a response to a certain disease state.
|
Need To Know: Some causes of a fast heart rate are:
|
Fast heartbeats that originate above the ventricles – in the
Types of SVTs are:
- Sinus tachycardia (fast heartbeat but with normal rhythm)
- Atrial tachycardia (fast heartbeat originating in the upper chamber of the heart)
Atrial fibrillation Atrial flutter - Some types of fast heart rates that involve the AV node
These relatively common rhythms are not usually serious – but they can cause considerable discomfort. Individuals often describe a feeling of a racing or pounding heart. Others experience light-headedness, shortness of breath, or weakness.
The rhythm usually starts and stops suddenly, however, and it only requires treatment if symptoms occur often, last a long time, or are very bothersome.
|
Need To Know: Factors that are associated with an attack of SVT include:
|
Two supraventricular tachyarrhythmias that frequently occur at the same time and that sometimes require treatment are:
- Atrial fibrillation
- Atrial flutter
Individuals with atrial fibrillation have an irregular heartbeat that is typically too fast. Impulses are generated from multiple places in the atria instead of just from the
In contrast, individuals with atrial flutter have a regular, but very fast, heart rate of between 250 and 350 beats per minute.
Conditions often associated with these two types of arrhythmia include:
Coronary artery disease - Hypertension
- Mitral valve prolapse
- Congestive heart failure
- Rheumatic heart disease
- Cardiomyopathy
- Congenital atrial malformations
- Recent heart surgery
- Alcohol and drug use, especially withdrawal
- Chronic obstructive pulmonary disease
- Hyperthyroidism
|
Need To Know: Individuals with atrial fibrillation and atrial flutter may or may not experience symptoms. However, they are more susceptible to developing blood clots because these chambers cannot completely empty between heartbeats, allowing the remaining blood to become stagnant. Blood clots in the heart can break off and block small Therefore, people with atrial fibrillation or atrial flutter often need to take anticoagulant drugs (“blood-thinners”). These medications do not actually thin the blood, but instead prevent the formation of blood clots. Some people also need treatment to control their heart rate or heart rhythm. |
Fast heartbeats that originate in the ventricles are called
- Palpitations
- Shortness of breath
- Light-headedness
Individuals with fast heart rates (faster than 180 beats per minute) and underlying heart disease are more susceptible to loss of consciousness (syncope) due to reduced blood pressure, and even sudden death.
|
Need To Know: The most dangerous form of ventricular tachycardia is called ventricular fibrillation. In this condition, multiple sites in the ventricle fire impulses rapidly and in an uncoordinated manner, causing the ventricles to quiver and stop pumping blood effectively. Unless a normal rhythm is promptly restored by emergency treatment, death occurs within several minutes. |
Most individuals with ventricular tachycardias have underlying heart disease (such as coronary artery disease or valve disease). But certain drugs and electrolyte (salts in the blood) disturbances also contribute to ventricular tachyarrhythmias.
Palpitations Associated With A Slow Heart Rate
A slow heart rate of less than 60 beats per minute is known as bradycardia (from the Greek word for slow). The two mechanisms that lead to slow heart rates are:
- Failure of the sinus node to generate impulses (sinus bradycardia)
- Failure of the impulses to be to conducted normally to the ventricles (AV block)
Bradycardia can be found in well-trained athletes as well as other individuals in excellent health. Normally, these individuals do not experience symptoms, and the slow heart rate is no reason for concern. Bradycardia also can be caused by vomiting, an underactive thyroid gland, or certain medications.
|
Need To Know: Some causes of a slow heart rate
|
In some people, however, a slow heart rate may mean that there is a problem with the heart’s electrical system. The problem could be:
- Sick sinus syndrome, in which the number of functional cells in the sinus node is decreased due to disease or advanced age. This is the most common cause of bradyarrhythmias.
- A variant of
sick sinus syndrome , known as bradycardia-tachycardia syndrome, which involves alternating bouts of a slow and fast heart rate. Heart block (AV block), in which impulses from the atria are delayed (first-degree block), intermittently blocked (second-degree block) or completely blocked (third-degree block) from reaching the ventricles.
The need for treatment is based on the site of the AV block as well as the degree of symptoms. Whereas young people and those in good cardiovascular health may tolerate slow heart rates, older people and those with even mild heart disease may experience symptoms of inadequate blood flow including:
- Dizziness
- Weakness
- Fainting
- Fatigue
- Shortness of breath.
Syncope (loss of consciousness) and death also may occur. A
How Are Palpitations Diagnosed?
When you tell your doctor about the palpitations, you will likely be asked a number of questions, such as:
- How often the palpitations occur
- How long they last
- What circumstances bring on the palpitations
- Whether other symptoms occur with the palpitations.
The doctor will then perform a physical examination to look for signs of conditions that may be causing your palpitations.
Your doctor can order a variety of tests to determine whether your palpitations are due to an abnormal heart rhythm. Some of these tests evaluate the heart’s chambers, valves, and arteries. Others focus primarily on the heart’s electrical system.
|
How-To Information: Ways in which your doctor can evaluate your palpitations:
|
Routine Electrocardiography
Routine or standard electrocardiography is the most commonly performed test in cardiology. This painless and harmless test produces an electrocardiogram (ECG or EKG) , which is a record of the electrical activity of the heart.
In this test, surface electrodes attached to wires (leads) are applied to the skin of your chest and limbs. These leads send your heart’s electrical signals to the electrocardiograph machine, which records this information on paper. The ECG shows a series of waves that represent the electrical events of various chambers and the conduction pathways within the heart.
A standard 12-lead ECG can diagnose disturbances in the heart rate or rhythm associated with palpitations, but only if palpitations occur while the ECG is being obtained. In addition to recording the heart’s rhythm, the ECG may help to identify an underlying cardiac condition, such as thickening of the heart muscle due to high blood pressure, disease of the heart valve, or a previous heart attack (myocardial infarction).
For further information about high blood pressure, go to high blood pressure.
For further information about heart attack, go to heart attack.
Long-Term ECG Recording
Individuals with suspected heart rhythm irregularities that are not recorded on a routine ECG will often undergo some type of home or ambulatory ECG monitoring. These methods include 24-hour Holter monitoring, transtelephonic event recording, and continuous loop recording.

- Holter monitor – A Holter monitor is a portable ECG recorder that you wear for 24 hours to obtain a continuous recording of your heart’s electrical activity. The ECG is recorded on a tape or computer chip and later analyzed by a computer for interpretation by your doctor. Several electrodes are placed on your chest and are connected by wires to a small recorder.
This recorder can be worn on a strap over your shoulder or around your waist while you continue with your normal daily activities. You will be asked to keep a diary while wearing the recorder so correlations may be made between your palpitations and the associated rhythm.
- Event (transtelephonic) recorders – If you do not feel
palpitations very often, you may be given a machine called an event recorder to keep with you. Event recorders are small devices that record short ECG intervals and are not intended to be worn all of the time.When you start to feel palpitations, you take it out and attach the device to your body temporarily. You do this by putting on a bracelet that attaches to the recorder or by pressing the device against your chest. You then press a button that initiates recording of your heart rhythm for up to one minute. The ECG is then transmitted by telephone to your doctor’s office for interpretation.
- Loop recorders – A continuous loop recorder is an ECG recorder applied to the surface of the skin that records several minutes of electrical activity at a time. It continuously records new information while discarding old information, so its memory stores only several minutes worth of information. But you can “freeze” the recording in the device’s memory if you experience palpitations.
As with event recorders, you transmit information recorded on a computer chip to your doctor’s office by telephone. These devices are useful for capturing brief episodes of electrical activity when it takes too long to apply an event recorder.
|
Nice To Know: An implantable form of a continuous loop recorder, known as an implantable loop recorder (IRL), may be implanted under the skin. These devices require no external electrodes or power source and use a small hand-held activator to “freeze” ECG information surrounding an event. |
Signal-Averaged ECG
This noninvasive test produces a surface ECG that allows your doctor to detect areas of slowed ventricular activation. This test is useful in determining whether an individual is at risk for ventricular
Exercise ECG (Stress Test)
In this test, an electrocardiograph machine records your heart’s electrical activity while you increase your heart rate by walking on a treadmill. This allows doctors to study changes in your ECG while your heart is made to work harder.
A stress test can show if the arteries that supply blood to the heart are partially blocked, as may occur with
Echocardiography
An ultrasound probe is placed on your chest and sound waves are directed through the probe to your heart. A computer shows images of the heart on a video screen by “reading” echoes of the sound waves as they bounce off the heart. This procedure does not involve any exposure to radiation and is painless.
Chest X-ray

The chest x-ray is an examination that employs a beam of energy (ionizing radiation) to obtain images of the heart, lungs, and ribs. It allows a physician to view the size of the heart and may reveal underlying heart or lung problems that could be linked to the palpitations.
Blood Tests
On occasion, a sample of blood is taken for specific laboratory tests. These tests can identify or rule out chemical causes of rhythm disturbances, such as an overactive or underactive thyroid gland, anemia, kidney problems, or abnormal levels of sodium, potassium, calcium, or magnesium.
Other Tests
Some more invasive tests involve the use of thin tubes called catheters, which are inserted into a blood vessel, usually near the groin. These catheters then are guided up through the blood vessels to the heart. The following two tests are performed at the hospital and may require an overnight stay.
Cardiac catheterization provides information about the anatomic structures of the heart as well as pressures inside the heart chambers. This test is useful for diagnosing various cardiac conditions that may be associated with arrhythmias.A dye can be injected through the catheters that allow the arteries of the heart to be seen on an X-ray film and checked for blockages seen with coronary artery disease. Dye can also be injected into the heart’s pumping chambers to see how well the heart muscle is contracting and the valves are working.
- An electrophysiologic (EP) study is used when spontaneous arrhythmias are infrequent but when a serious
arrhythmia is suspected. This test involves inserting wires (electrode catheters) into leg, arm, or neckveins and guiding them into the heart using x-ray.In addition to obtaining information about electrical events from various locations in the heart, these catheters can serve as pacemakers and allow the doctor to stimulate the heart to produce a change in heart rhythm. This can allow the doctor to observe the portion of the heart involved in producing the arrhythmia. This test is useful in identifying abnormal circuits (electrical pathways) in the heart, which can then be destroyed with radiofrequency energy so the arrhythmia will not recur. The area that is destroyed is very small.
How Are Palpitations Treated?
In most people, palpitations do not indicate underlying heart disease, and treatment other than reassurance or lifestyle changes is not needed. In some cases, your doctor may discover that your palpitations are due to an arrhythmia (irregular heartbeat) that warrants medical treatment. Several types of treatments are available for palpitations caused by problems with heart rate or heart rhythm.
Common Medications
The basic treatment for the management of most important arrhythmias are medications called “antiarrhythmics.” These agents are generally classified according to their mechanism of action. There are four classes of these medications:
- Class I antiarrhythmic drugs, known as “sodium channel blockers.” These medications have long been used in the United States to control arrhythmias. They work by blocking “sodium channels” (the transport of sodium across the cell walls) in order to slow impulse conduction in the heart.
But these agents can also depress function in the left ventricle (reduce effectiveness of pumping) and aggravate or promote arrhythmias. Some of these induced arrhythmias are serious, so these drugs should always be used with caution.
|
Nice To Know: Examples of Class I antiarrhythmic drugs are:
|
- Class II antiarrhythmic drugs, known as “beta-blockers.” These medications slow the heart rate and force of contraction by decreasing the sensitivity of cells to
adrenaline and adrenaline-like substances that act at beta receptors. Beta-blockers have long been used to control supraventricular tachycardias (SVTs), and recent evidence suggests they may be helpful in suppressing ventriculartachycardia and ventricular fibrillation.Although beta-blockers can also cause
bradycardia , these induced arrhythmias are generally not serious. Other side effects of beta-blockers include left ventricular depression, fatigue, and stomach upset. Beta-blockers are also used to treat high blood pressure and angina (chest pain that occurs when thearteries do not supply enough blood to the heart). They are commonly used after a heart attack.
|
Nice To Know: Examples of Class II antiarrhythmic drugs are:
|
- Class III antiarrhythmic drugs, known as “potassium channel blockers.” They work, in part, by prolonging the recovery time of cardiac cells after they have carried an impulse. This can prevent circuits (electrical pathways) from causing an arrhythmia or only permit slower arrhythmias.
|
Nice To Know: Examples of Class III antiarrhythmic drugs are:
|
- Class IV antiarrhythmic drugs, known as “calcium channel blockers.” These medications slow the heart rate by blocking heart cells’ calcium channels (transport of calcium across the cell walls) and slowing conduction at the AV node.
In addition to slowing the heart rate, these medications dilate (open up) blood vessels and decrease the force of cardiac contraction. Like beta-blockers, calcium channel blockers are used to control some forms of SVT and ventricular tachycardia and to slow the ventricular rate in people with atrial fibrillation.
|
Nice To Know: Examples of Class IV antiarrhythmic drugs are:
|
Other Medications
In addition to the above four classes of antiarrhythmic drugs, there are also some miscellaneous drugs:
- Digoxin – This medication increases the strength of heart muscle contractions and is useful in the treatment of heart failure. Because digoxin also slows conduction through the AV node, it may be useful in controlling atrial fibrillation, atrial flutter, and atrial tachycardia. It often is combined with beta- or calcium-channel blockers.
- Adenosine – This drug slows or blocks conduction through the AV node by acting on special adenosine receptors. Since adenosine is only available in intravenous form and only works for a short time, it is only used as acute treatment for supraventricular tachycardias.
Pacemakers
A
The pacemaker is generally implanted under the skin, just beneath the collarbone. Most people go home the same day following the implant, but some need an overnight hospital stay.
Artificial pacemakers are the most commonly used treatment for a slow heart rate (bradycardia). Pacemakers work by sensing electrical signals from the heart and sending out electrical impulses for a slow heart rate, to cause the heart to beat if the heart does not generate an electrical impulse after a certain period of time.
Pacemakers for a fast heartbeat also exist. These implantable pacemakers are about the size of conventional pacemakers and are used to automatically stop certain fast arrhythmias.
Electrical Cardioversion And Defibrillation
In cardioversion, an electric shock is delivered to the heart to stop an abnormal rhythm and allow a normal rhythm to resume. This shock is applied through two paddles on the chest, or one on the chest and one on the back. The electric shock interrupts the heartbeat for a brief moment. This resets the heart’s electrical control system and can return the heart to a normal rhythm.
Cardioversion is used to stop all life-threatening tachycardias. The conversion of ventricular fibrillation to sinus rhythm is referred to as defibrillation. Cardioversion is also useful for stopping supraventricular tachycardias such as atrial flutter or atrial fibrillation.
Radiofrequency (Catheter) Ablation
Radiofrequency (catheter) ablation refers to the destruction of small portions of electrical pathways in the heart using long, thin, plastic-coated wires (catheters). This catheters are threaded through the blood vessels to the heart, much like the
After the circuit has been mapped, electrical energy is delivered to the tip of the wire. This energy causes a small burn at the site of the catheter tip, which destroys the circuit. This technique has revolutionized the treatment of many arrhythmias and is considered to be quite safe.
Implantable Cardioverter-Defibrillators (ICDs)
For some individuals (such as those with frequent, poorly controlled ventricular tachycardia, or people with a history of resuscitated sudden death), a small automatic device can be surgically implanted under the collarbone to deliver an electric shock to the heart if a serious arrhythmia is detected. Such a system is referred to as an implantable cardioverter-defibrillator, or ICD. As these systems do not prevent arrhythmias, they are combined with other therapy that suppresses arrhythmias.
What to Do For Palpitations

If you experience palpitations, remember that most are not life threatening and are not caused by a serious problem.
If your doctor has determined that they are not due to a serious cause, here’s what you can do when they happen.
- Lie down and try to remain calm. Panic can aggravate the problem.
- Splash cold water on your face.
- Exhale forcefully, as if you are trying to blow up a balloon.
Lifestyle Changes
It’s best to check with your doctor if you experience palpitations. If your palpitations do not happen often, do not last long, are not accompanied by other symptoms, and do not appear to be due to underlying heart disease or serious
- Get regular exercise. Try to walk for 20 or 30 minutes, three to five days a week. Start slowly and gradually build up your speed. Check with your doctor if you are considering an activity more vigorous than walking
- Cut down on caffeine. Drink less coffee and black tea, and avoid food that contains caffeine, such as chocolate.
- Get more sleep.
- If you are under stress, consider a stress management program, therapeutic massage, yoga, or any other activity to help you relax.
Keeping Track Of Your Palpitations
If you start getting palpitations more often, or if they last longer, keep track of information that can help your doctor determine the cause, such as:
- What were you doing at the times you felt palpitations?
- What did you eat or drink before you started feeling the palpitations?
- Were you experiencing stress?
- Were you exercising?
- If you are a woman, do your palpitations seem linked to your menstrual cycle?
Palpitations: Frequently Asked Questions
Here are some frequently asked questions related to palpitations.
Q: My doctor says I need to take medicine for my palpitations, but I’ve heard that they can have side effects. Should I be concerned?
A: Almost all medications have some side effects and that includes antiarrhythmic drugs. Fortunately, most of the side effects of antiarrhythmic drugs are not serious at usual doses. But you should ask about any possible serious side effects of the medication you’re taking, and report any side effects to your doctor. In some cases, this may require discontinuation of the medication. However, if you can’t take one type of medicine because of side effects, chances are good that a different medication can help you. To avoid problems with medication interactions, be sure to tell your doctor about all other medications you are taking.
Q: I need a
A: Modern pacemakers are not affected by microwave ovens. However, certain types of electrical fields still can disturb them (for example, MRI procedures or cellular telephones). Your doctor will tell you what potential sources of electromagnetic energy you should avoid.
Q: I just had a routine EKG (electrocardiogram), and my doctor told me I have
A: It’s not uncommon for some people with a slow heart rate caused by heart block to have no symptoms. In many cases, the problem is discovered with routine tests.
Q: Every once in a while, I could swear that my heart actually skips a beat. Can this be harmful in the long run?
A: A feeling of skipped heartbeats is a very common description of palpitations. In most cases, it has nothing to do with how well your heart is performing. You are especially likely to notice skipped heartbeats if you are tired or have had too much caffeine or alcohol.
Q: Sometimes it feels like my heart is beating very slowly, then suddenly it feels as if it’s beating too quickly. What could be wrong?
A: Sometimes, people with a variant of
Palpitations: Putting It All Together
Here is a summary of the important facts and information related to palpitations.
- Palpitations are a sensation that the heart is beating rapidly, slowly, forcefully, or irregularly.
- The majority of palpitations are not of major significance and are not a sign of underlying heart disease. They are more common as you get older.
- If your palpitations do not happen often and do not last long, you can make changes in your lifestyle that may help to stop or reduce them.
- If your palpitations happen more than once a week, last more than a half minute, or are associated with other symptoms such as sweating, chest pain, shortness of breath, dizziness, or fainting, your should see your doctor.
- Often, your doctor can rule out serious problems through a physical examination and simple tests. Occasionally, other tests such as
cardiac catheterization are needed. - Treatments available for conditions that cause palpitations include medications, catheter ablation, the use of an artificial
pacemaker or implanted defibrillator, and cardioversion/defibrillation.
Palpitations: Glossary
Here are definitions of medical terms related to palpitations.
Adrenaline: One of the chemical messengers in the body that causes the heart to beat faster.
Arrhythmia: Any rhythm that is not the normal rhythm of the heart; it may mean a slow or fast heart rate or an irregular rhythm.
Arteries: The blood vessels that carry blood away from the heart and around the body.
Atria: The two upper chambers of the heart (the left atrium and the right atrium), which take in blood from the veins.
Atrial fibrillation: A condition in which the heartbeat is irregular and often rapid
Atrial flutter: A condition in which the upper chambers of the heart contract rapidly but regularly.
AV (atrioventricular) node: A relay station between the atria and ventricles that causes a delay in the electrical impulse to permit the atria to finish contracting (emptying) before ventricular contraction
Bradycardia: A slow heart rate (less than about 60 beats per minute).
Cardiac catheterization: A procedure in which thin tubes are threaded through the blood vessels to the heart to detect blockages indicative of coronary artery disease. This test is also used to see how well the heart muscle contracts and the valves function.
Catecholamines: Chemical messengers in the body that send signals to the sinus node to increase the heart rate; one such catecholamine is adrenaline (epinephrine).
Coronary artery disease: Blockages of the arteries that supply blood to the heart muscle.
Echocardiography: A noninvasive test that uses sound waves to produce images of the heart on a monitor.
Ectopic beats (extrasystoles): The term used to describe a short sequence of extra heartbeats (premature contractions).
Electrocardiogram (ECG or EKG): A recording of the electrical activity of the heart.
Heart block: A condition in which the impulses from the heart’s upper chambers are delayed or blocked from reaching the lower chambers.
Normal sinus rhythm: The normal rhythm of the heart.
Pacemaker: An electrical device that delivers electrical impulses to produce a heartbeat of desired frequency. Implantable pacemakers are the mainstay of treatment for bradycardia, and are also useful for sometachycardias.
Palpitations: Awareness of the heart beating; the heartbeat may feel fast, slow, forceful, or irregular.
Sick sinus syndrome: A disorder in the heart’s sinus node that affects how heartbeats are generated and how they are conducted. It usually causes a slow heart rate that may cause a person to faint. A related disorder is bradycardia-tachycardia syndrome, which involves alternating bouts of fast and slow rhythms.
Sinus node: The body’s natural “pacemaker,” which lies in the heart’s right atrium and generates a rhythm of electrical impulses to cause the heart muscle to contract.
SVTs (supraventricular tachycardias): Fast heartbeats that originate above the ventricles (in the atria, AV node, or both).
Tachycardia: The term used to describe a rapid heartbeat of greater than 100 beats per minute.
Veins: The blood vessels that carry blood back to the heart.
Ventricles: The two lower chambers of the heart (the left ventricle and the right ventricle), which pump blood out of the heart and into the arteries.
Ventricular tachyarrhythmias: Fast heartbeats that originate in the ventricles.
Palpitations: Additional Sources Of Information
Here are some reliable sources that can provide more information on palpitations.
- Mitral valve prolapse, a deformity of one of the heart’s four valves, is another heart-related cause of palpitations. If your palpitations are due to mitral valve prolapse (MVP), you may want to visit the MVPS Research and Support Web site at http://www.mvpsupport.com, for more information as well as stories from people with this condition.
